-
PDF
- Split View
-
Views
-
Cite
Cite
Georgia R Layton, Marinos Koulouroudias, Eyad Issa, Steve Jepson, Antonio F Corno, Ashley R Dennison, Unligated vertical vein presenting as a large atrio-portal shunt in adulthood: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa377, https://doi.org/10.1093/jscr/rjaa377
Close - Share Icon Share
Abstract
A 28-year-old male with infra-cardiac totally anomalous pulmonary venous connection (TAPVC) repaired as new-born presented in adulthood with right heart strain and very large left atrium to portal vein vessel. Residual connections from pulmonary veins to systemic circulation are believed to represent persistent ‘vertical veins’ (VV) not ligated at the time of the initial surgery. In our patient, since endovascular occlusion was not judged suitable, the anomalous vessel was surgically ligated and resected. A review of the literature failed to find such a procedure reported in an adult patient and analyzed the intra-operative ligation of VV during repair of TAPVC.
INTRODUCTION
Totally anomalous pulmonary venous connection (TAPVC) is a congenital defect characterized by incomplete development of all pulmonary veins, which instead of connecting to the left atrium (LA) drain into systemic veins. The infra-cardiac variation is associated with the confluence of all pulmonary veins, which, through a descending vertical vein (VV) passing behind the LA, drain sub-diaphragmatically into splanchnic veins. This defect commonly presents in neonates with right heart failure and pulmonary venous obstruction [1]. There is variation in the surgical approach to the VV during repair of TAPVC; a number of published cases report persistent enlargement of the VV when flow through a VV is maintained at the time of repair. This frequently results in cardiovascular compromise during childhood, with a significant number of patients requiring delayed intervention [2–4]. Interval closure can often be achieved endovascularly, however, this is the first case of open surgical repair in adulthood of a large shunt representing a persistent VV due to contra-indications to endovascular repair.
CASE REPORT
At 3-weeks old, this patient had presented critically ill with congestive heart failure necessitating emergent repair of congenital infra-cardiac TAPVC through sternotomy, deep hypothermia and circulatory arrest, with direct anastomosis of the pulmonary venous confluence (PVC) to the posterior wall of the LA and closure of a patent foramen ovale. The VV was intentionally maintained patent. Recovery proceeded uneventfully, and he was discharged home on the sixth post-operative day. Regular reviews were performed throughout childhood without issue or evidence of residual shunting.
Surveillance MRI was performed together with exercise testing at 25 years of age and excluded any focal pulmonary vein stenosis. The right ventricle was dilated, but with preserved systolic function (EF = 49%) and the portal vein, connected with the LA and the common pulmonary vein confluence, which was dilated. A triple-phase computed tomography (CT) scan (Fig. 1A) demonstrated a large vessel connecting the postero-inferior aspect of the LA and the mid-point of the portal vein. A CT scan with 3D reconstruction was performed to further clarify the anatomy (Fig. 1B).
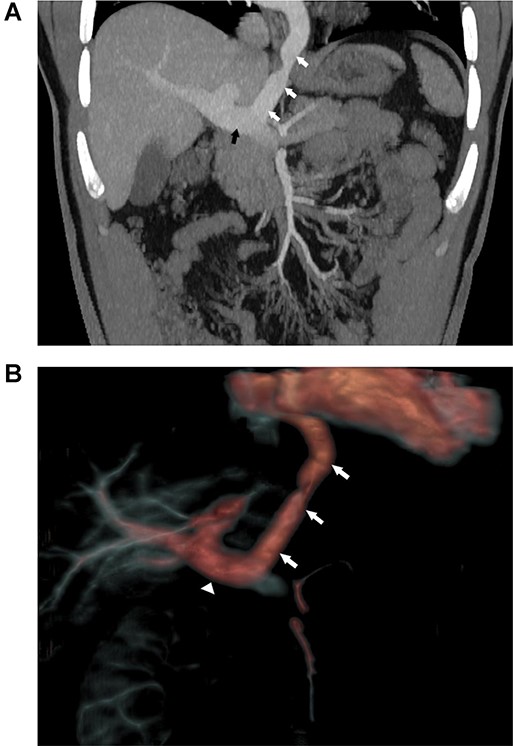
(A) Coronal view of abdominal CT with contrast demonstrating the large vessel (white arrows) between LA and portal vein (black arrow). (B) 3D reconstruction of CT with contrast demonstrating the large vessel (arrows) between LA and portal vein (triangle).
The findings were discussed at the congenital cardiac multi-disciplinary team (MDT) meeting. Closure via endovascular approach was judged unsafe because of size and length of the intra-abdominal component and therefore a referral was made to the regional tertiary hepatobiliary team.
At 28-years old, a transverse laparotomy was performed in the mid-upper abdomen, the hepato-duodenal ligament was opened to expose the portal vein and the remnant VV was identified (Fig. 2). The vessel was occluded with vascular clamps and hemodynamic parameters were closely monitored. Since clamp occlusion did not produce any variation of the hemodynamic status or cardiac electrophysiology, the proximal aspect of the vessel was divided at the level of the diaphragm using an Echelon Flex™ (Ethicon, USA) vascular stapler. The distal end was subsequently ligated at the portal vein using 3-0 absorbable ties and over-sewn with 4-0 non-absorbable monofilament. The vessel was fully excised.
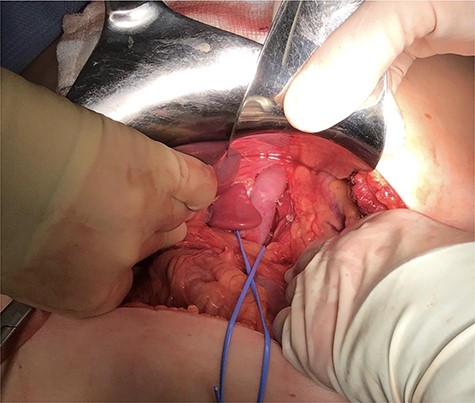
Intra-abdominal exposure of the infra-diaphragmatic portion of the vessel following ligation of a small left lateral tributary.
No post-operative complications were observed, and the patient was discharged home on the fifth post-operative day. Telephone follow-up was conducted at 8 weeks when the patient reported complete healing of his laparotomy wound and good exercise tolerance.
DISCUSSION
There remains equipoise in respect of whether the VV should be ligated or left patent during initial TAPVC repair surgery. Zhao et al. describe a 26-year experience of TAPVC repair, demonstrating excellent survival with 92.6% of patients alive at 5 years. The VV was ligated in 57 patients and left patent in 20 when left atrial pressure was >15 mmHg following occlusion of the vein intra-operatively. One patient developed significant left-to-right shunt necessitating endovascular closure of the patent VV [5]. Leaving the VV patent at the initial operation provides a reservoir for the poorly compliant left-heart chambers frequently present in the setting of obstructed TAPVC [6]. The long-term sequalae of allowing this acute off-loading of the LA remains unknown, and although it may be beneficial during the early post-operative phase, continued patency of the VV is likely to result in a progressive left-to-right shunt requiring interval intervention to prevent congestive heart failure [7].
Cope et al. reviewed a series of patients subsequent to 1986 when they had ceased VV ligation. Their main finding was that non-ligation of the VV led to lower pump runs and during long term follow-up, flow was found to be abolished in the VV. Furthermore, in patients with obstructed TAPVC, all deaths occurred in patients where the VV was ligated during the initial corrective procedure [8]. The hypothesis that the VV will eventually obliterate was challenged by Kumar et al. who found that in patients with an unligated VV, left-to-right shunting of blood in the vein persisted even when catheterization demonstrated low pressure in the LA and absence of obstruction at the level of the anastomosis between PVC and LA [2]. A number of possible explanations for failure of closure of the VV after TAPVC repair have been suggested but it is now believed to be secondary to either preferential flow into the LA or high resistance to flow through the hepatic parenchyma [6, 9].
A trans-septal, endovascular approach is the most commonly reported method of shunt closure. This may be precluded by technical issues relating to specific anatomical configuration or institutional experience which may be insufficient to confidently perform this procedure. Given the size of the vessel in our patient, we were concerned that occlusion without resection of the remnant vessel could result in the formation of collaterals, thrombosis or recanalization and recurrence. A trans-abdominal approach to a large descending VV has never been previously reported. However, the use of voluminous and large lumen devices required for vessels as large as the one in our patient increases the risks of transcatheter closure [10]. When patients present with a persistent VV, considerable anatomical variation is described, treatment options are complex, and complications are associated with significant morbidity. Due to the rarity of this condition, it is impossible to be dogmatic about the management. Each patient should be treated on their own merit after discussion and expert consensus by a specialist congenital heart disease MDT.
AUTHOR’S STATEMENT
Written permission was granted by the patient to publish the case and associated figures. All authors provided significant contribution to, and final approval of, this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



