-
PDF
- Split View
-
Views
-
Cite
Cite
Paul Ghaly, Glen Schlaphoff, John Crozier, Mehtab Ahmad, Upper limb phlegmasia cerulea dolens treated with single-session suction thrombectomy: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa364, https://doi.org/10.1093/jscr/rjaa364
Close - Share Icon Share
Abstract
Phlegmasia cerulea dolens (PCD) of the lower limbs is a rare condition. PCD of the upper limbs is extremely uncommon, with only a select few cases documented in the literature. A complication of severe deep venous thrombosis, PCD, is characterized by the clinical triad of oedema, pain and limb cyanosis. Delays in treatment are associated with high rates of morbidity and mortality. We present a case of sudden-onset upper limb PCD in a 68-year-old man following haemodialysis through a long-term arteriovenous fistula. Prompt diagnosis and rapid initiation of intravenous anticoagulation followed by urgent single-session suction thrombectomy resulted in the successful restoration of vessel patency without any significant adverse sequelae on 3-month follow-up.
INTRODUCTION
Acute upper limb deep vein thrombosis (DVT) is an uncommon clinical presentation, whilst upper limb phlegmasia cerulea dolens (PCD) is even rarer [1]. PCD describes a clinical syndrome characterized by a triad of acute limb swelling, pain and cyanosis (or purple discolouration) of the affected limb. PCD is a consequence of severe DVT resulting in complete venous obstruction impeding venous return, leading to fluid extravasation and limb oedema. An interplay of Virchow’s triad, risk factors for PCD include hypercoagulable states such as malignancy, venous stasis and trauma. It is a potentially critical condition with complications including venous gangrene, limb loss and death [1–3]. Prompt recognition and institution of mainstay therapies is paramount to the alleviation of thrombus burden and overall improvement in patient outcomes.
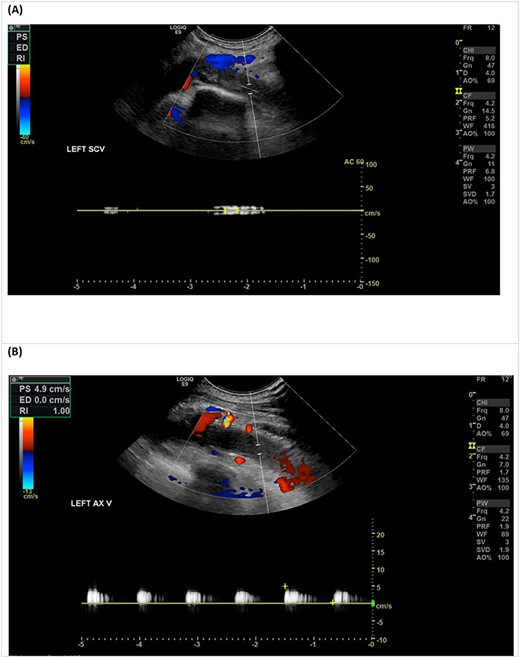
Venous duplex ultrasound of the LUL demonstrating an occlusive thrombus in the left subclavian vein (A), with sluggish flow in the axillary vein (B).
CASE REPORT
A 68-year-old man with a history of end-stage renal failure requiring haemodialysis (HD) secondary to diabetic nephropathy was admitted with acute left upper limb (LUL) swelling following successful completion of a HD session through a left forearm radio-cephalic arteriovenous fistula (RC-AVF) created 4 years prior. He reported experiencing pain in his left arm 2 days prior to presentation, however denied any obvious limb swelling. On completion of his outpatient HD session, marked swelling of his LUL extending to the shoulder was noted, prompting emergency referral to vascular surgery. His medications included aspirin and clopidogrel as dual anti-platelet therapy (DAPT) and atorvastatin and isosorbide mononitrate for hypercholesterolaemia and ischaemic heart disease, respectively.
On examination, his vital signs were unremarkable—heart rate 67 beats per minute, blood pressure 124/73 mmHg, respiratory rate 18 breaths/min and oxygen saturations of 98% on room air. Visual inspection of the LUL revealed significant pitting oedema and purple discolouration from the shoulder to the fingers. The LUL was cool to touch in comparison to the right; however, distal pulses remained palpable. An audible bruit was evident on auscultation of the RC-AVF, but no thrill was palpable. There was no evidence of objectively decreased sensation over the LUL, and power was recorded as 4/5 in all movements of the affected limb, with a normal neurovascular examination in the other extremities.
An urgent duplex ultrasound study demonstrated cephalic vein outflow obstruction with occlusive thrombus in the proximal left subclavian/axillary vein confluence (Fig. 1). The basilic vein at the level of the proximal forearm remained patent. He was immediately given a bolus of intravenous unfractionated heparin (UFH) and commenced on a UFH infusion, with a plan for urgent venous thrombectomy.
Thrombectomy was performed using the JETi Thrombectomy System™ (Walk Vascular LLC, CA, USA) of the left subclavian vein thrombus within 24 hours of symptom onset. Post-thrombectomy venogram demonstrated good restoration of flow; however, a short proximal subclavian vein stenosis was identified and treated with 8 × 40 mm balloon venoplasty. A good venographic result was seen on completion (Fig. 2).
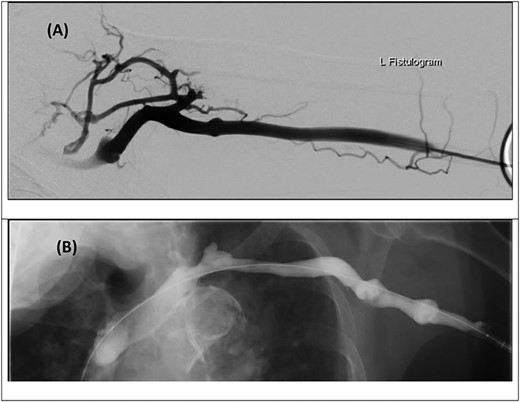
Digital subtraction venogram images prior to thrombectomy demonstrating occlusive thrombus at the proximal left subclavian vein/axillary vein confluence with numerous collateral vessels within the shoulder and axilla (A and B). (C) Post-thrombectomy venogram demonstrating improved flow with no further collateral vessels noted.
The following day his LUL swelling had markedly reduced and the purple discolouration completely resolved. He underwent his usual HD protocol through the left RC-AVF 24-hour post-procedure without any complications. He was commenced on warfarin for long-term anticoagulation in addition to DAPT and continued on an UFH infusion whilst bridging to warfarinization. He was discharged on post-operative Day 5 and duplex imaging at 30 days and on 3-month follow-up demonstrated continued patency of all LUL vessels.
DISCUSSION
PCD is a rare entity associated with a high morbidity and mortality rate. It results from extensive proximal venous outflow obstruction in the setting of minimal venous tributary collateralization, resulting in venous gangrene and/or limb loss. PCD is characterized by four cardinal signs: oedema, pain, limb cyanosis and extreme venous outflow obstruction. In contrast to the insidious onset of symptomatic DVT, PCD symptoms evolve rapidly over hours [1–3]. Untreated PCD is fatal in 25-40% of cases and the reported rate of amputation in survivors is 20–50% [4, 5]. Aetiology includes malignancy, trauma (e.g. venous catheterization procedures and surgery), heparin-induced thrombocytopenia, antiphospholipid syndrome and pregnancy [2–4].
Current management strategies for the treatment of PCD in both the upper and lower limbs are derived from those for iliofemoral DVT, given the rare nature of presentation. Treatment involves a combination of medical therapies, such as anticoagulation and thrombolytic therapy and surgical interventions such as catheter-directed thrombolysis (CDT) or percutaneous thrombectomy.
Prompt initiation of therapeutic anticoagulation is used to halt thrombus progression and propagation. Despite the effectiveness of CDT, its utility is marred by other considerations such as the need for prolonged infusion times (24–72 hours), the need for enhanced nursing care and monitoring in a high-dependency unit or intensive care unit setting and the associated risks of catheter-site or systemic haemorrhage. Percutaneous mechanical thrombectomy offers the advantage of rapid thrombus removal without the accompanying risks of thrombolytic therapy.
The successful outcome of our case can be attributed to several factors. The onset of symptoms whilst the patient was attending his HD ensured prompt referral to our vascular unit for review. Additionally, familiarity with the patient’s upper limb vasculature from the time of his RC-AVF creation aided diagnosis. Furthermore, prompt initiation of treatment with UFH and early restoration of blood flow minimized the associated complications of PCD.
CONCLUSION
PCD of the upper limbs is a rare condition that requires time-sensitive intervention for positive patient outcomes. Recognition of the clinical entity amongst physicians, particularly emergency and primary care clinicians can ensure early referral to secondary specialist care and treatment, thus minimizing its associated morbidity and mortality.
CONFLICT OF INTEREST STATEMENT
None declared.



