-
PDF
- Split View
-
Views
-
Cite
Cite
Majd Abouassi, Mohammad Aloulou, Nouran Hawa, Tayf Toutounji, Safwan Alyousef, Successful eradication of a large orbital hydatid cyst without rupture using fronto-orbitozygomatic approach, the first case reported from Syria, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa357, https://doi.org/10.1093/jscr/rjaa357
Close - Share Icon Share
Abstract
Hydatid disease is a parasitic infection resulted by Echinococcus granulosus in the larval stage and is most prevalent in the Middle East, India, Africa, South America, New Zealand, Australia, Turkey and Southern Europe. However, orbital hydatid cysts are rare and represent a challenge to the surgeon to eradicate the cyst without rupture. Here, we report a case of a relatively large primary intraconal orbital cyst in a 21-year-old woman. We managed to eradicate the cyst without any complication using fronto-orbitozygomatic approach, and the patient remained disease free after the 3 months of follow-up.
INTRODUCTION
Echinococcus granulosus causes the hydatid disease, which is endemic in the Middle East, India, Africa, South America, New Zealand, Australia, Turkey and Southern Europe [1–4]. It commonly locates in the liver, lungs and abdominal cavity. However, orbital hydatid cysts are rare, accounting for <1% of the hydatid cysts [2–6]. Patients usually present with proptosis, chemosis, ocular motility disturbance and visual impairment [3].
Here, we report a case of a young woman presented with continuous, not-responding-to-analgesics headache, preceding the ophthalmic symptoms. She was then diagnosed with a relatively large intraconal orbital hydatid cyst that was removed surgically using fronto-orbitozygomatic approach without rupture.

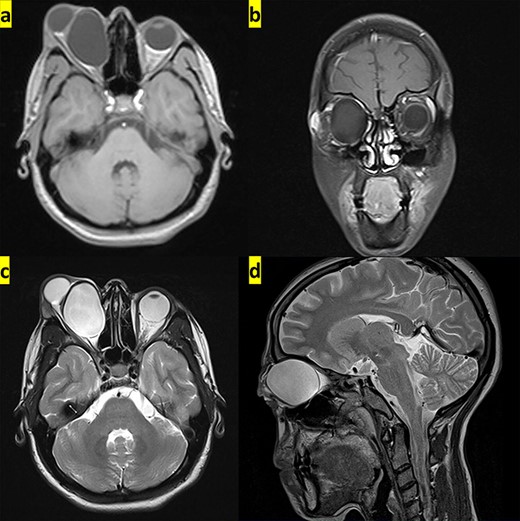
The transverse and coronal planes from MRI show hypointense hydatid cyst on T1-weighted images (a and b), whereas it appears hyperintense in the transverse and sagittal planes from MRI on T2-weighted images (c and d).

CASE PRESENTATION
A 21-year-old Caucasian woman was admitted to the neurosurgery department with severe visual impairment and proptosis in the right eye. About 9 months earlier, she was suffering from a headache on the right side of the head, which caused sleeping difficulty. Four months later, the patient noticed right-sided proptosis, but she did not ask for medical consultation for fear that the surgical intervention might affect her pregnancy at that time. The patient lives in a rural area in contact with dogs and sheep. Her past medical history was unremarkable.
On physical examination, the patient was conscious, responsive and oriented. Visual acuity was only a perception of light in the right eye, and there was a complete restriction in this eye movement with severe chemosis (Fig. 1). The exophthalmia was non-axial, painless, non-tender, irreducible and non-pulsative. Magnetic resonance imaging (MRI) revealed a well-defined cystic lesion that measures ∼42 × 36 × 32 mm, located in the right orbital cavity displacing the optic nerve laterally. The lesion showed low signal intensity on T1-weighted images (Fig. 2a and b) and high signal intensity on T2-weighted images (Fig. 2c and d).
The diagnosis was an intraconal orbital hydatid cyst. Chest X-ray and abdominal ultrasonography revealed no abnormal findings, and there were no other abnormalities in the general examination. In addition, the left eye and laboratory tests were normal.
Ophthalmic consultation recommended eradication via a neurosurgical approach due to the risk of rupture because of the large size. The patient underwent surgery using fronto-orbitozygomatic approach in which we made an incision in the right frontal skin and removed the right orbitozygomatic bony flap. Then, we opened the roof of the orbit and removed the hydatid cyst successfully without rupture (Fig. 3).
During the surgery, the eye returned to the orbital cavity spontaneously, and the proptosis disappeared in the immediate postoperative period. On the first day after surgery, the patient was conscious with severe eyelid edema treated with dexamethasone. On the third day, the edema was subsided, and there was a noticeable improvement in the visual ability from a perception of light to the ability to count fingers at a distance of 1 m. The patient was discharged after 72 hours of the surgical procedure with a prescription of antibiotic, analgesic, antiedemic and albendazole (10 mg\kg once daily for 2 months). There was no clinical recurrence of proptosis after the 3 months of follow-up (Fig. 4), and her eye motility and vision returned to normal.

After the 3 months of follow-up, the proptosis and chemosis disappeared, and the eye movements returned to normal.
DISCUSSION
Hydatid cyst is a parasitic infection resulted by E. granulosus; the majority of cysts are found in organs like the liver and lungs, whereas the worldwide incidence of orbital hydatid cysts is 1% of all cysts [7]. However, it accounts for 19.8% in endemic countries [8]. Xiao and Xueyi [4] surveyed 3736 cases of hydatid cyst; 18 of them were orbital cysts, which accounts for 0.3%.
Although Syria is an endemic country, our case is the first documented orbital hydatid cyst from our country.
In these literature reviews [1, 2, 4, 7], the age of the patients ranges between 15 and 20 years, and this agrees to our patient age, which is 21 years old.
Superolateral and superomedial angles of the orbital cavity or close to the muscle con are the most common sites of orbital hydatid cyst [2, 8].
Besides, the incidence in the left orbit is more common than the right one [8].
Our patient had an intraconal cyst in the right orbital cavity, obscuring medial rectus muscle, compressing optic nerve laterally.
Ordinary orbital hydatid cyst tends to be unilateral and slowly progressive. It also causes proptosis, pain, visual loss and other ocular symptoms [9].
The initial symptom of our patient was a not-responding-to-analgesics headache. Four months later, the right eye proptosis and the partial visual loss started to develop.
Orbital hydatid cysts usually spread from another area of the body through the portal and systematic circulation and are then known as secondary cysts, whereas primary cysts in the orbit cavity without other organ involvement are rare [1, 10].
In our case, the cyst is a primary one in which Echinococcus directly settled in the orbital cavity without other organ involvement.
MRI and computerized tomography (CT) are the most used diagnostic methods, whereas the accurate diagnosis in some patients can be made only histopathologically during the surgical intervention [1].
Surgery is the curative treatment for such cases, in which a complete removal of the cyst is done. However, it is usually complicated by rupture due to the anatomical complexity of the orbital cavity and the restricted surgical area [10].
However, we managed to eradicate the cyst without any complication using fronto-orbitozygomatic approach.
In order to minimize recurrence, albendazole is useful, especially if used 14–28 days before the surgery [9].
We prescribed albendazole (10 mg\kg once daily for 2 months) to our patient after the surgical procedure, and she remained disease free after the 3 months of follow-up.
CONCLUSION
Hydatid cysts should be taken into consideration as a differential diagnosis of unilateral proptosis in patients from countries where hydatidosis is endemic.
In addition, early diagnosis of the lesion is essential, because the delay in the diagnosis allows the cyst to grow in size and represents a challenge to the surgeon to eradicate it without rupture.
CONSENT
Written informed consent was obtained from the patient for publishing this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal on request.
AUTHORS CONTRIBUTIONS
M.A, M.A, N.H, T.T: Conception and design, data analysis and interpretation, drafting, revision. S.A: The Supervisors, patient care, revising critically. All authors discussed the content of the manuscript, read and approved the final manuscript.
ACKNOWLEDGEMENTS
Authors are grateful to CME office at the faculty of medicine, University of Aleppo, Aleppo, Syria, for the efforts and support (cme.office@alepuniv.edu.sy).
CONFLICT OF INTEREST STATEMENT
None declared.



