-
PDF
- Split View
-
Views
-
Cite
Cite
Omar Marghich, Alexandre Maubert, Efoé-Ga Yawod Olivier Amouzou, Louis Denimal, Emmanuel Benizri, Mohammed Amine Rahili, Idiopathic small bowel diaphragm disease: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa358, https://doi.org/10.1093/jscr/rjaa358
Close - Share Icon Share
Abstract
Small bowel diaphragm disease is a rare condition usually associated with the prolonged use of non-steroidal anti-inflammatory drugs (NSAID) and that can be mistaken and treated as other pathologies. We describe a case of a 64-year-old man with a prolonged course of pain and subacute bowel obstructions, without any history of NSAID usage, found to have a multiple diaphragmatic stricture in the small bowel.
INTRODUCTION
Small bowel diaphragm (SBD) disease, first described by Lang et al. [1] in the late 1980s, is a rare condition usually associated to the prolonged use of non-steroidal anti-inflammatory drugs (NSAID) and characterized by the presence of multiple diaphragm-like septa that cause the narrowing of the small bowel lumen. Most cases are asymptomatic until they present with acute intestinal obstruction [2]. It is a condition that is difficult to diagnose both preoperatively and intraoperatively. Herein, we describe the case of a 64-year-old man with a prolonged course of pain and subacute bowel obstructions, without any history of NSAID usage, found to have a multiple diaphragmatic stricture in the small bowel.
CASE PRESENTATION
On the initial admission, the 64-year-old man had a 1-year history of chronic intermittent abdominal pain and episodes of subacute bowel obstruction. The patient had no history of chronic medication usage.
Initial investigations included magnetic resonance enterography that was normal and a capsule endoscopy that showed rare erosions, aphthoid ulcers and two ulcerated stenosis (Fig. 1).

One month later, he developed an acute small bowel obstruction, and a laparotomy was therefore undertaken.
The laparotomy revealed the presence of two transition zones between dilated and non-dilated small bowel. These zones were located within 40 cm proximal to the ileocecal valve, and they corresponded to a few millimeters thin lesions, with no evidence of a thickening in the bowel or mesenteric abnormalities (classic stigmata of stenotic Crohn disease). An enterotomy for one of the two lesions was undertaken, which showed no macroscopic abnormality, and then a stricturoplasty was made.
A diagnosis of ileal Crohn disease was suspected leading to the initiation of a treatment with biotherapy (adalimumab).
A second capsule endoscopy showed the same lesions.
One year later, he was readmitted with small bowel obstruction investigated with an abdominal computed tomography (CT) scan that showed no radiological finding of stenotic Crohn disease or other obstructive etiology (Figs 2 and 3).
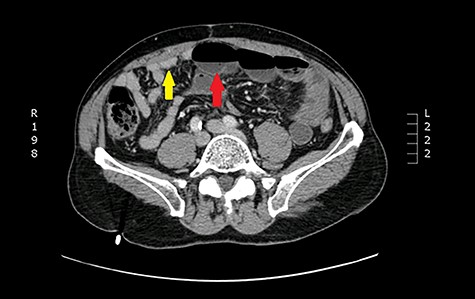
Axial view: arrows pointing to dilated and collapsed small bowel.
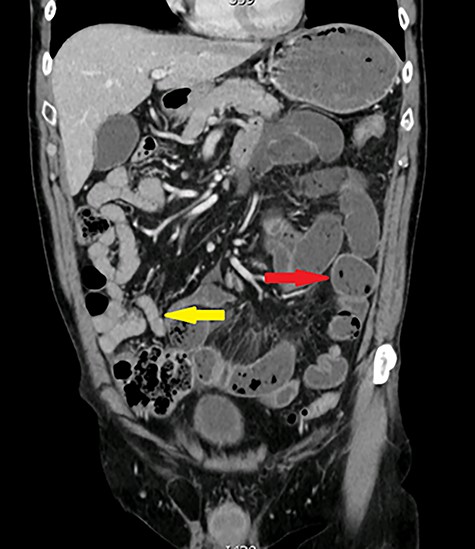
Coronal view: arrows pointing to dilated and collapsed small bowel.
The small bowel occlusion was resolved with non-operative management.
After a multidisciplinary team discussion, an exploratory laparoscopy was decided in order to explore the extraluminal aspects at the obstruction area and execute an enteroscopy in order to ensure the existence of intraluminal unique or multiple lesions.
At laparoscopy, the patient was found to have stigmata from the previous operation without any other extraluminal anomalies on the small bowel or the mesenteric fat. A conversion to a mini-laparotomy was undertaken, and using manual palpation, 2 mm thin strictures were suspected to be the possible zones of the small bowel obstacle.
No other particular anomalies were perceived and a small enterotomy was performed 35 cm above the Bauhin valve near the previous stricturoplasty. The peroperative enteroscopy reached proximally the duodeno-jejunal angle and distally the ileocaecal valve and the caecum allowing the exploration of the entire small bowel (Fig. 4). It showed multiple ileal diaphragm including three diaphragms with small ulcers (video). A 60 cm segmental resection was performed removing all the six lesions and the histological features found in the lesion were consistent with the diaphragm disease.

DISCUSSION
SBD disease, first described by Lang et al. [1] in the late 1980s, is a rare condition. While the long-term use of NSAIDs is considered the single most important causative factor of SBD, many other medications, diseases and processes may cause injuries to the small bowel and result in strictures of the small bowel lumen, such as potassium chloride tablets, surgical anastomoses, radiation, ischemia, Crohn disease, tuberculosis, eosinophilic enteritis, lymphoma, etc [3–7].
The disease process of SBD does not affect the full thickness of the bowel and is predominantly found in the ileum. Although rarer, it has also been reported to affect the colon [3].
Most cases are asymptomatic until they present with acute intestinal obstruction. Other presenting features are iron-deficient anemia, acute hemorrhage and an acute abdomen secondary to perforation [2, 3, 5]
CT scan and endoscopic techniques are commonly used in preoperative diagnosis; however, CT scanning tends to lack the resolution required to highlight the SBD and generally do not show any abnormal results when used to explore chronic abdominal pain, and it could advocate for small bowel acute strangulation on adhesions when used to explore acute small bowel occlusion [8–10]. In regards to capsule enteroscopy, it should only be undertaken on patients with iron-deficiency anemia with no obstructive symptoms, to prevent the risk of capsule retention [3–6].
On the other hand, surgical intervention generally does not show any extraluminal abnormalities on the small bowel or the mesenteric fat, which leads to an enterotomy. This enterotomy frequently shows no abnormal mucosa, and generally leads to a stricturoplasty for its closure without a good knowledge of the diagnosis.
In contrast, our observation advocates for the role of peroperative enteroscopy in detecting the SBD that could be unique or multiple, which can reduce the small bowel lumen and be responsible for chronic abdominal pain and recurrent small bowel obstructions.
Histological features of the lesions are thickening and chaotic arrangement of muscular bundles in the muscularis mucosae, fibrosis of the lamina propriae, invariable mucosal ulceration at the apex of the diaphragm, numerous vessels, ganglion cells, nerve fibers and eosinophils in the mucosa [9].
Surgical intervention remains the treatment of choice and will usually involve resection of the affected segment. In cases of extensive or recurrent disease stricturoplasty may be preferred [4]. In some cases the disease can affect the entire length of the small bowel, and it may be that some residual disease has to be left after the initial resection of the lesions.
CONCLUSION
This case report is an additional new case of SBD. It confirms that:
The disease is difficult to diagnosis, can be mistaken and treated as other pathologies.
Should be considered in case of recurrent bowel obstruction and chronic abdominal pain.
Surgical intervention associated with intraoperative enteroscopy remains the treatment of choice.
These lesions could occur without a history of chronic NSAID usage.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



