-
PDF
- Split View
-
Views
-
Cite
Cite
Ryohei Takei, Masashi Hashimoto, Ryosuke Zaimoku, Hirohumi Terakawa, Itsuro Terada, Yuji Tsukioka, Masato Kiriyama, Pedicled jejunal flap reconstruction for partial duodenectomy: a report of two cases, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa296, https://doi.org/10.1093/jscr/rjaa296
Close - Share Icon Share
Abstract
Conventional jejunal reconstruction procedures for large duodenal defects include jejunal serosal patch repair and duodenojejunostomy and have some risks of postoperative complications. The pedicled jejunal flap is used for reconstruction following laryngopharyngectomy, esophagectomy and other gastrointestinal surgeries. We report two cases of successful closure of duodenal defects after partial duodenectomies by pedicled jejunal flap reconstruction. Case 1: A 72-year-old man was diagnosed with gastrointestinal stromal tumor by esophagogastroduodenoscopy (EGD), endoscopic ultrasound-guided fine needle aspiration biopsy and computed tomography (CT). Case 2: A 63-year-old woman was diagnosed with early duodenal cancer using EGD and CT. Partial duodenectomy and pedicled jejunal flap reconstruction were performed in both patients. A part of the jejunum was formed into a pedicled flap to fit the duodenal defect and duodenojejunal anastomosis was performed. The patients did not report any postoperative gastrointestinal symptoms or abnormal findings during follow-up EGD or upper gastrointestinal radiography.
INTRODUCTION
Gastrointestinal surgeons sometimes find it difficult to repair a large duodenal defect caused by a severe perforating duodenal ulcer or by partial duodenectomy for duodenal tumors. Repairing procedures for duodenal defects include simple closure, jejunal serosal patch repair and duodenojejunostomy (Roux-en-Y anastomosis). These procedures have risks of duodenal stenosis, internal hernia and blind loop syndrome. Jejunal reconstruction is performed for various surgical procedures such as laryngopharyngectomy, esophagectomy and other gastrointestinal surgeries [1, 2]. Here, we report two cases of successful pedicled jejunal flap reconstruction for partial duodenectomy.
CASE REPORT
Case 1
A 72-year-old man was found to have a duodenal tumor on complete medical examination. Esophagogastroduodenoscopy (EGD) showed a submucosal-like mass (1.5 × 1.5 cm) on the opposite side of the duodenal papilla (Fig. 1a). Endoscopic ultrasound (EUS) revealed a tumor derived from the muscular layer of the duodenal wall (Fig. 1b). Computed tomography (CT) showed an enhanced tumor (1.5 × 1.7 cm) in the descending part of the duodenum without lymph node metastasis or distant metastasis (Fig. 1c). The pathological diagnosis of the fine needle aspiration biopsy samples was a gastrointestinal stromal tumor (GIST) (Fig. 1d). We performed partial duodenectomy and pedicled jejunal flap reconstruction for a 6 × 8 cm duodenal defect (Fig. 2a). A part of the jejunum at a distance of 30–40 cm from the ligament of Treitz was isolated and formed into a pedicled flap to fit the duodenal defect (Fig. 2b). The jejunal flap was passed through the retro-colic route, and duodenojejunal anastomosis was performed using an Albert–Lembert suture (Fig. 2c and d). In addition to the jejunojejunal anastomosis, we closed the space between the mesentery of the colon and jejunal flap. The pathological diagnosis of the resected specimen was the same as that of the preoperative diagnosis. The patient was discharged on the 11th postoperative day without any surgical complications. No tumor recurrence or gastrointestinal symptoms were reported 13 months after surgery.
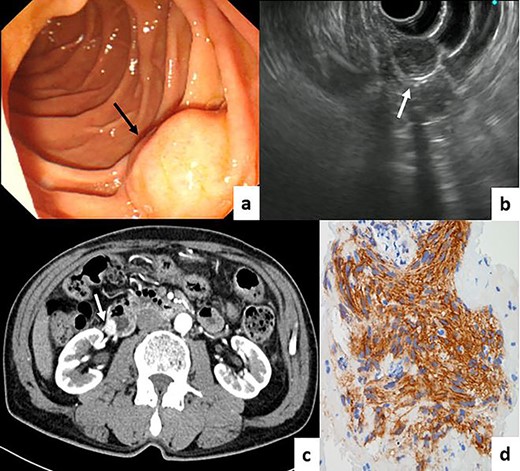
(a) EGD showed a submucosal-like mass on the opposite side of the duodenal papilla (black arrow). (b) EUS revealed a tumor derived from the muscular layer of the duodenal wall (white arrow). (c) CT showing an enhanced tumor in the descending part of the duodenum. (d) Immunohistochemical assessment of the fine needle aspiration biopsy samples showing the GIST (KIT ×400).
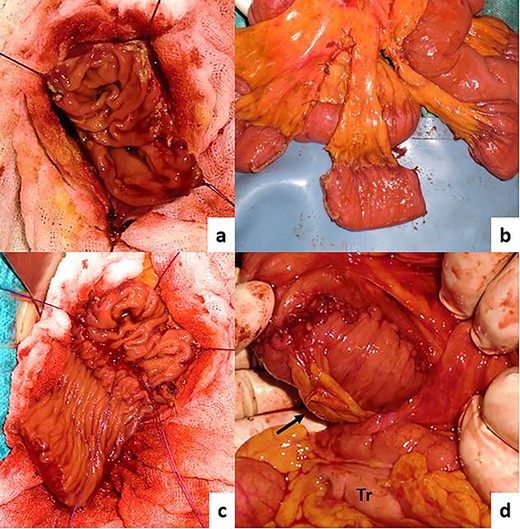
Intraoperative images. (a) Partial duodenectomy, (b) pedicled jejunal flap formation, (c) anastomosis, (d) finished reconstruction. The jejunal flap was passed through the retro-colic route (jejunal pedicle: black arrow, transverse colon: Tr).
Case 2
A 63-year-old woman was found to have a 7 × 8 mm, 0–IIc type tumor on the opposite side of the duodenal papilla in the follow-up EGD after endoscopic submucosal dissection for early gastric cancer (Fig. 3a). The pathological diagnosis was well-differentiated adenocarcinoma (Fig. 3b). CT revealed no lymph node metastasis or distant metastasis (Fig. 3c). We diagnosed early duodenal cancer as cT1aN0M0 (TNM classification). We planned to perform partial duodenectomy first and then pancreatoduodenectomy secondarily if the pathological examination of the resected specimen showed advanced duodenal cancer. After the duodenectomy, pedicled jejunal flap reconstruction was performed in the same manner as in Case 1. The pathological diagnosis was early duodenal cancer (pTisN0M0Stage0). The patient was discharged on the ninth postoperative day without any surgical complications. No tumor recurrence or gastrointestinal symptoms were reported 14 months after surgery. Follow-up EGD and upper gastrointestinal radiography did not show any signs of stenosis or motility disorder (Fig. 4a and b).
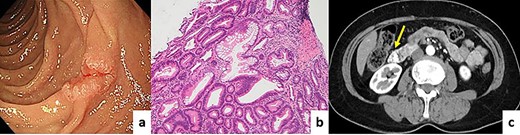
(a) EGD showing a 0–IIc type tumor on the opposite side of the duodenal papilla. (b) Pathological diagnosis was well-differentiated adenocarcinoma (hematoxylin and eosin ×40). (c) CT revealed some clips taken after tumor biopsy as a hyperdense area.
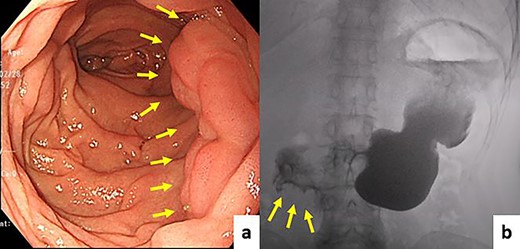
Follow-up EGD and upper gastrointestinal radiography did not show stenosis, diverticulum, or motility disorder. (a) EGD, (b) upper gastrointestinal radiography.
DISCUSSION
Pedicled jejunum is used in the form of an interposition or flap for reconstruction following laryngopharyngectomy, esophagectomy and other gastrointestinal surgeries. Only a few cases of pedicled jejunal flap reconstruction for duodenal defects have been reported [3, 4]. Simple closure, jejunal serosal patch repair and duodenojejunostomy (Roux-en-Y anastomosis) have been performed to repair duodenal defects. However, these procedures have risks of duodenal stenosis, internal hernia and blind loop syndrome. Pedicled jejunal flap reconstruction has many advantages compared with conventional procedures. Firstly, foods pass physiologically and the patient has a lower risk of postoperative ileus due to internal hernia as it is not necessary to make significant changes in the functioning of the digestive tract. Secondly, it is possible to close even a larger duodenal defect by forming a large flap [5]. Thirdly, pedicled jejunal flap repair leads to better wound healing of the defect than the serosal patch [6]. Finally, in a situation like Case 2, a two-step pancreatoduodenectomy is easier to perform than the other procedures. On the other hand, postoperative failure and flap necrosis due to the ischemia is the specific complication of this procedure.
When performing pedicled jejunal flap reconstruction, attention should be paid to the direction of the intestinal peristalsis and flap size. A too small or too large flap induces duodenal stenosis or diverticulum at the anastomotic site. In both of our cases, duodenal stenosis, diverticulum and motility disorder were not observed on follow-up EGD or upper gastrointestinal radiography. We think it is also important to confirm good blood flow of the flap using intraoperative Doppler ultrasonography in some high-risk cases to prevent postoperative failure and flap necrosis [7].
Herein, we report two cases of successful closure of a duodenal defect after a partial duodenectomy using pedicled jejunal flap reconstruction. In cases where gastrointestinal surgeons may have trouble closing a large duodenal defect caused by a severe perforating duodenal ulcer and partial duodenectomy for a benign tumor or early carcinoma, pedicled jejunal flap reconstruction would be useful. More cases with long-term follow-up data would be needed to complement the success of this procedure.
ACKNOWLEDGMENTS
The authors would like to thank Editage (www.editage.com) for English language editing.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
REFERENCES
- diagnostic radiologic examination
- computed tomography
- biopsy
- postoperative complications
- upper gastrointestinal endoscopy
- anastomosis, surgical
- esophagectomy
- follow-up
- reconstructive surgical procedures
- signs and symptoms, digestive
- duodenum
- malignant neoplasm of duodenum
- jejunum
- gastrointestinal stromal tumor
- gastrointestinal surgical procedures
- laryngopharyngectomy
- duodenojejunostomy
- duodenectomy
- endoscopic ultrasound-guided fine needle aspiration
- jejunal serosal patch



