-
PDF
- Split View
-
Views
-
Cite
Cite
David Z Allen, Rishabh Sethia, Erin Hamersley, Charles A Elmaraghy, Presentation of an iatrogenically displaced third molar into the maxillary sinus in a 14-year-old patient successfully removed with an endoscopic approach: a case report and a review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa290, https://doi.org/10.1093/jscr/rjaa290
Close - Share Icon Share
Abstract
Oral surgeons remove third molars (wisdom teeth) to prevent impaction. Given the close anatomical relationship to the maxillary sinus, perforation and displacement of third molars into the maxillary sinus is a well-known phenomenon that is typically removed with a buccal mucoperiosteal flap or through a Caldwell–Luc approach. However, a less invasive route of endoscopic removal has been utilized to success in one report. A literature review shows few reports of displaced molars into the maxillary sinus and no reported patient below the age of 18. A 14-year-old patient presented with a displaced third molar into her maxillary sinus following third molar extraction with her oral surgeon. The tooth was removed successfully, utilizing endoscopic sinus surgery (ESS) with a transition to transoral retrieval to prevent nasal trauma. This is the first reported case of displaced third molar into the right maxillary sinus in a pediatric patient that was removed via ESS.
INTRODUCTION
Third molar, or wisdom teeth, extractions are common operations that typically occur in young adulthood [1]. While low risk, third molar extractions do have complications such alveolar osteitis, abscess and hematoma formation [1]. A well-known, but poorly reported, complication is displacement of the third molar into the maxillary sinus during extraction given the adjacent anatomic relationship between the maxillary sinus and the superior premolars and molars [2–5]. While multiple reasons exist for displacement, a known risk factor is the use of excessive force with the elevator instrument during extraction [6]. Though these displacements can be asymptomatic, some complain of chronic sinusitis, facial swelling and trismus and thus removal is indicated [5].
In general, there exists a gap in the literature detailing incidence of iatrogenic displacement into the maxillary sinus. Specifically, there are no reports of displaced maxillary teeth in pediatric patients (the youngest patient is 18 years old). Published reports describe surgical removal via a Caldwell–Luc or buccal mucoperiosteal flap [3]. Due to the invasive nature of these approaches and multiple surgical fields, an endoscopic approach has been suggested and utilized in one adult [6]. Due to the lack of literature, further discussion of third molar displacement and intervention is necessary, especially in pediatrics.
We share our experience with a 14-year-old female who presented with her parents requesting removal of a displaced tooth into the maxillary sinus after a tooth extraction. This tooth was successfully removed endoscopically.
CASE REPORT
A 14-year-old female patient with no significant past medical history presented to our department 11 days following third molar extraction during which tooth number one was displaced into the right maxillary sinus cavity. A complete history and physical was performed. The patient was asymptomatic with postoperative changes along her gingiva, but the remainder of her exam was normal. There was no sinus tenderness reported on palpation or signs of sinusitis on endoscopy. A computed tomography (CT) scan of the sinuses without contrast was performed, which revealed the displaced molar within the posterior inferior maxillary sinus and a posterior maxillary wall defect (arrow, Fig. 1A and B).
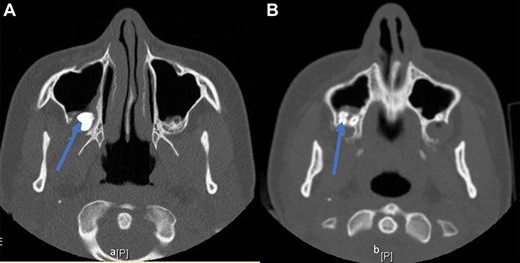
(A, B) CT sinus images of a displaced third molar (arrow) into the posterior aspect of the maxillary right sinus.
After identifying the location of the displaced tooth, the recommendation was made for removal. After reviewing the risks, benefits and indications for the procedure, the parents consented to removal of the tooth using right-sided ESS carried out under image guidance.
Decongestion and anesthetic were applied to the nose, the right middle turbinate was medialized, and the uncinate was removed using ball tip probe and backbiting forceps in preparation for right maxillary antrostomy. The natural maxillary ostium was enlarged for maxillary antrostomy. Once the antrostomy was complete, the molar was visualized in the posterior, inferior sinus cavity consistent with imaging. It was grasped with Blakesley forceps after several attempts secondary to smooth texture, size and location (Fig. 2). The tooth was pulled into the right nasal cavity but was too large to extract anteriorly through the naris. To prevent trauma to the nasal passageway, the tooth was pushed posteriorly into the nasopharynx and extracted via a transoral approach using a Crowe–Davis retractor and hemostat.
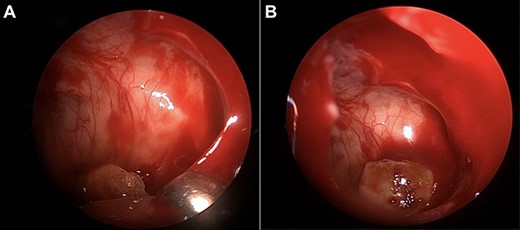
(A, B) intraoperative images of the third molar removal from the maxillary sinus.
Following the removal, the sinonasal cavity was irrigated with saline. Absorbable hemostat was applied to achieve hemostasis. The patient tolerated the operation well and was discharged same day.
DISCUSSION
Third molars are common and can lead to cyst formation if impacted [7]. In order to treat impacted teeth, extraction is performed [1, 8]. While generally well tolerated, there exists risk for complications [1]. Specifically, there is possibility for displacement of a molar into the maxillary sinus, particularly if excessive force is used intraoperatively [6]. Perforations of the maxillary sinus can also occur during extraction given the proximity of the teeth to the sinus [8]. There is limited literature describing reports of iatrogenically displaced teeth into the maxillary sinus and none in patients under 18 years old.
Of the published reports, the patients present for removal variable after the extraction [2, 3]. While some of the patients were asymptomatic, others complained of sinus tenderness, infection and chronic sinusitis. Most patients required surgical removal [6, 9]. Historically the surgical approach utilized for removal of displaced teeth into the maxillary sinus has included an antrostomy via a buccal gingiva–mucosal periosteal flap or a trans-antral route [10]. These approaches are invasive routes of removal and require separate surgical fields. Thus, a less traumatic route of removal is a worthwhile consideration.
ESS is utilized for multiple pathologies in the sinonasal cavity and has been utilized successfully in the past for removal of foreign bodies [5]. However, there has only been one report that detailed an endoscopic removal of an iatrogenically displaced third molar into the maxillary sinus [9].
Our case successfully utilized an endoscopic approach with maxillary antrostomy for removal of the tooth (Fig. 2A and B). We did remove the tooth from the patient via a final transoral route to prevent injury to the nasal cavity secondary to the size of the nasal cavity, which required pushing the tooth into the nasopharynx. This endoscopic extraction and transoral retrieval is different than prior reports and worked well in a pediatric patient. Providers may consider a transoral approach for final retrieval of the tooth in pediatric patients with narrow nasal cavities.
CONCLUSION
We present the first case of endoscopic removal of an iatrogenically displaced third molar into the maxillary sinus in a pediatric patient. This case report adds to the literature describing successful utilization of an endoscopic approach for removal of displaced teeth into the sinuses. Ultimate transition to a transoral removal of the tooth allowed for removal of a large molar from a pediatric patient without further traumatizing the anterior nasal cavity. This combined endoscopic and transoral removal is less invasive than the previously described trans-antral operations. We recommend consideration of endoscopic and possibly combined transoral retrieval of displaced teeth into the maxillary sinus in pediatric patients.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DISCLAIMER
The views expressed in this article reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the United States Government.



