-
PDF
- Split View
-
Views
-
Cite
Cite
Ntenis Nerntengian, Grigorios Gkasdaris, Theodosios Birbilis, Clipping of a basilar tip aneurysm using hypothermia and circulatory arrest: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa262, https://doi.org/10.1093/jscr/rjaa262
Close - Share Icon Share
Abstract
Treatment of complex and giant aneurysms remains challenging despite modern endovascular and microsurgical techniques. We report the first case of microsurgical clipping of a complex basilar tip aneurysm under circulatory arrest and hypothermia performed in Greece. A 52-year-old patient presented with a Hunt and Hess Grade 4 subarachnoid hemorrhage. The digital subtraction angiography revealed a complex basilar tip aneurysm. Due to aneurysm complexity, we decided for microsurgical clipping under hypothermia and circulatory arrest. We performed a right pterional craniotomy with orbitozygomatic osteotomy. The patient was then put on heart–lung-machine. Following hypothermia and circulatory arrest, the aneurysm was clipped with its complete occlusion. The patient was discharged with no neurological deficits. Clipping of complex aneurysms under hypothermia and cardiac arrest performed by experienced team is a safe alternative when endovascular therapy or bypass technique is not feasible.
INTRODUCTION
Despite the rapid technological developments in the field of endovascular therapy and the improvements of microsurgical techniques, complex and giant aneurysms without clearly defined neck and in surgically difficult to access anatomical regions pose a great challenge for a definitive treatment with good results. In recent decades, certain high-volume neurosurgical centers utilize circulatory arrest and profound hypothermia during microsurgical clipping of complex aneurysms with promising results [1–3]. In this article, we report the first case of microsurgical clipping of complex basilar tip aneurysm with employment of hypothermia and circulatory arrest performed in Greece [4].
CASE REPORT
A 52-year-old patient was admitted to our hospital with a subarachnoid hemorrhage Hunt and Hess Grade 4 (Fig. 1). The digital subtraction angiography (DSA) revealed a complex basilar tip aneurysm (Fig. 2A). At the time of patient’s presentation in our clinic, there was no endovascular therapy option in our institution as our hospital lacked a neurointerventional infrastructure. As the optimal timing of surgically treating high-grade aneurysmal subarachnoidal hemorrhage is still controversial and our patient presented with hydrocephalus and a Hunt and Hess Grade 4 subarachnoidal hemorrhage, we first decided to treat the hydrocephalus with placement of an external ventricular drainage. The anatomical location of the aneurysm in the narrow space of interpeduncular fossa filled with blood clots and the severe brain edema were additional factors to the poor initial clinical presentation of the patient that made us decide for a delayed surgical treatment. Under intensive care therapy and treatment of the hydrocephalus with the external ventricular drainage, the clinical situation of the patient improved to Hunt and Hess Grade 3 preoperatively. We decided to clip the aneurysm under hypothermia and temporarycardiac arrest as the wide neck of the aneurysm, its large size and the narrow surgical space could not ensure the safe preparation of the aneurysm neck and the surrounding vessels and would also require a prolonged temporary clip application with increased ischemia risk if a technique with temporarily deflating the aneurysmal sac and allowing comfortable surgical maneuvres was not used. We conducted a thorough preoperative cardiological evaluation that revealed no contraindication for application of extracorporeal circulation using the heart–lung-machine. The operation took place 14 days after the rupture of the aneurysm. The surgical approach was done via a right-sided pterional craniotomy combined with orbitozygomatic osteotomy. Then, the sylvian fissure was opened; subsequently, the Liliequist membrane was opened through the optico-carotid cistern revealing the aneurysm. Following, a sternotomy and opening of the pericardium was performed by our cardiac surgeons. After intravenous administration of 35 000 IU heparin, an aortic and venous cannula was placed. The patient then was put on extracorporeal circulation with the use of heart–lung-machine and was cooled gradually down to 18°C (Fig. 3). At this point, a circulatory arrest was caused by stopping the heart–lung-machine. Simultaneously, the head of the operating table was elevated to promote emptying the blood from the aneurysm sac. Thanks to these manipulations, an efficient and comfortable microsurgical preparation of the aneurysm and its neck from the surrounding small perforating arteries and the proximal branches of the basilar artery was achieved. Hereafter, a clip was placed uneventfully occluding the aneurysm. We gradually rewarmed the patient up to 36.5°C in the following 15 minutes. After administration of protamine sulfate to antagonize the previously administered heparin, the surgery proceeded with the closure of the craniotomy and the thoracotomy. No postoperative complications were recorded and the patient was able to exit the intensive care unit in 8 weeks. A postoperative DSA confirmed the complete occlusion of the aneurysm (Fig. 2B). The patient was transferred 18 weeks after the operation with no focal neurological deficits at the referring hospital.

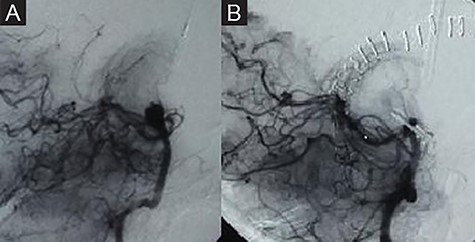
Preoperative DSA showing a complex basilar tip aneurysm (A). Complete occlusion of the aneurysm in the postoperative DSA (B).

Intraoperative image showing the synchronous surgical activity of neurosurgeons and the cardiac surgeons with the patient in extracorporeal circulation.
DISCUSSION
Although the use of hypothermia and cardiac arrest is part of the everyday routine for anesthesiologists who take part in cardiac surgeries [5–7], it is not free from risks and complications. The risk of cerebral ischemia increases the longer the cessation of circulation lasts. Because of this, a very reduced circulation instead of cardiac arrest is favored by many surgeons [2]. Hypothermia lowers the viscosity of the blood as well as the metabolism of glucose [8]. All of the above make the presence of an experienced anesthesiologist essential. An increased risk of postoperative bleeding, which has been reported [1], did not occur in our patient. With circulatory arrest for up to 30 minutes, the blood empties from the aneurysmal sac facilitating better and comfortable preparation of the neck of the aneurysm from the surrounding branches as well as an easier placement of the clip. Hypothermia reduces the metabolic needs of the brain and protects against possible ischemia [8]. The method can be applied in patients who do not have a preexisting cardiac risk factor, in aneurysms that cannot be treated endovascularly, extracranial to intracranial (EC–IC) bypass is not feasible, when the use of temporary clips is restricted by the anatomical features of the surgical area and if the aneurysm is complicated by branches that require a prolonged temporary clip application and microsurgical preparation carrying a risk of ischemic damage [3, 8]. According to our knowledge, this is the first case of complex aneurysm clipping with the aid of hypothermia and circulatory arrest in Greece. We believe that clipping of complex aneurysms using hypothermia and circulatory arrest when performed by experienced team of neurosurgeon, cardiac surgeon and anesthesiologist is a safe alternative when endovascular treatment and EC–IC bypass cannot be applied.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



