-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Saeed Falyoun, Qusai Mashlah, Qusai Aldiri, Ali Ramadan Mohamad, Lina Khalil Daowd, Malek Ayash, Epigastric heteropagus and omphalocele, Journal of Surgical Case Reports, Volume 2020, Issue 10, October 2020, rjaa437, https://doi.org/10.1093/jscr/rjaa437
Close - Share Icon Share
Abstract
We report a case of epigastric heteropagus twins with omphalocele. The parasite had two lower limbs, genitalia with developed phallus and scrotum but absent testis and absent anus. An omphalocele was present just below the attachment of the parasitic twin. No kidney or ureter but only a bladder filled with urine seen during exploration. The parasite bowel was attached to an omphalocele sac prolapsing through it and there was connection to the autosite liver, which forms the main source of its blood supply. Surgery was performed in the neonatal period (Day 12 after birth) for both excision of epigastric heteropagus and omphalocele repair.
INTRODUCTION
Conjoined twins can be symmetrical or asymmetrical (heteropagus). Heteropagus twins consist of the anatomically normal autosite and a parasitic twin that is incompletely formed.
CASE REPORT
This case report is of a male infant with normal spontaneous vaginal delivery, mother was 38 years old. She had been submitted to ultrasonography, and the malformation had not been identified. The child had an epigastric heteropagus twin (Figs 1 and 2). The parasite had two lower limbs and male genitalia with developed phallus and scrotum but absent testis and absent anus. The parasite was passing urine. The limbs did not move or respond to external stimulus. An omphalocele was present just below the attachment of the parasitic twin and the parasitic bowel was slightly prolapsing through it.
Echocardiography
Non-obstructive hypertrophic cardiomyopathy, ejection fraction (EF) 82%
Contrast enhanced computed tomography (CT): (Figs 3 and 4)
No obvious anomalies in the autosite viscera. No clear vascular or visceral contact between the twins. The parasite consists of pelvic and two femur bones with cystic formation may represent a bladder. A single pelvic kidney is suspected with some intestinal loops in the pelvis.
Surgical laparotomy
Circular incision was performed of the skin and subcutaneous tissue after taking sufficient skin from the parasite to ensure tension-free closure of the wound following separation. After that ligation was carried out of the parasitic urachus and mobilization its bladder. The pelvis of the heteropagus contained a bladder filled with urine with no kidney or ureter (Fig. 5). There was 25 cm of bowel that open on the sac of the omphalocele with a slightly prolapse (Fig. 6) without any connection to the autosite’s gut. Resection was performed of the omphalocele sac. The blood supply to the parasite is derived from the falciform ligament, separating the parasitic partition. The rest of autosite viscera was normal. Wound closure of autosite and umbilicoplasty are shown in Fig. 7.


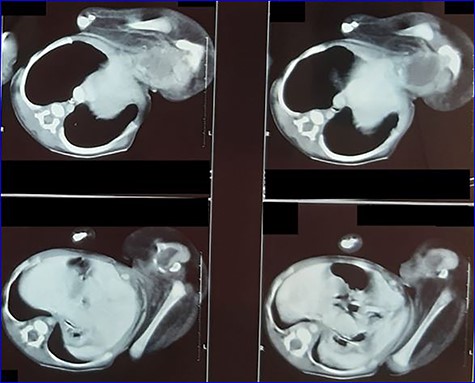
Contrast-enhanced CT scan image showing parasite’s viscera and bony parts.
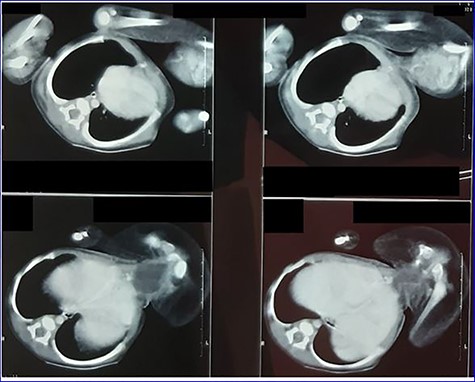
Contrast-enhanced CT scan image showing parasite’s viscera and bony parts.
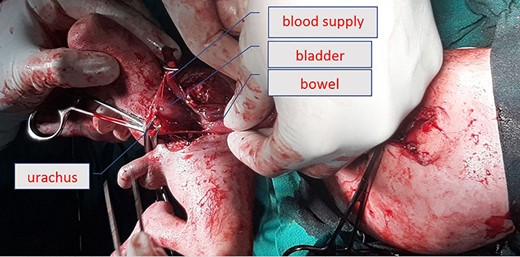
Operative picture showing blood supply and the bladder of parasite.


Our neonate withstood early surgery of epigastric heteropagus (EH) with omphalocele well, started oral feeding on the third day with good nutritional tolerance. Seven days after the surgery, there was dehiscence after wound infection. He was intubated and received parenteral nutrition. Then he acquired pneumonia. On the ninth day, he developed supraventricular tachycardia. Death occurred 40 days after the surgery because of respiratory distress and cardiac failure.
DISCUSSION
The incidence of conjoined twins is considered to be 1 in 50 000–100 000 births and is more commonly seen in females (70%). Heteropagus twins, however, are even rarer with an incidence of 0.05 to 0.1 in 100 000 births [1]. There is a male predominance in EH of 78% [2].
Only the caudal portion of the parasite develops. Rudimentary limbs, pelvis, external genitalia, genitourinary system and part of bowel are common anatomical structures developed in the parasite. The liver and rudimentary heart are other rare contents [3].
The limbs on the parasite do not move and are not sensate. There is absence of skeletal muscle in the limbs and this is thought to be due to the failure of myoblast differentiation attributable to lack of proper innervation. The parasite blood supply is derived from the autosite and this connection is evident during surgery. It can also be identified on preoperative CT or magnetic resonance imaging angiography. The most common blood supply to the parasite is derived from the falciform ligament. Other vessels that have been identified are left internal mammary, left subclavian, epigastric artery and left intrathoracic artery [1].
Omphalocele is the most common anomaly associated and followed by cardiac anomalies in the autosite. In the review of cases by Manish et al. [4] omphalocele was associated with EH in 50% of the cases.
In our case, the omphalocele was present and the parasite bowel was opening on the sac of the omphalocele with a slightly prolapse. The blood supply to the parasite is derived from the falciform ligament of the autosite. There was non-obstructive hypertrophic cardiomyopathy, EF 82%.
The sac with underlying adherent bowel prolapsing through it led us to go ahead with surgery in the neonatal period for both excision of EH and omphalocele repair. There are very few reported cases of emergency surgery or early separation and indication was either rupture of omphalocele or death of parasite twin. Early separation in neonatal period appears more beneficial as the tissues are more pliable and available for defect closure as in some of the reported cases, the death or devitalization of parasite occurs after birth. Moreover the late separation of EH with omphalocele results in loss of domain of peritoneal cavity as gut tends to occupy more space toward the omphalocele sac so chances of ventral hernia formation are increased.
Early separation also reduces the chances of intestinal obstruction or other bowel complications, if the parasite twin has bowel communication or adhesion with the autopagus bowel. Immediate exploration of an EH with a ruptured omphalocele has also been reported with no adverse complication.
In reviewing 86 articles detailing 106 pairs of heteropagus twins, 49 reported postoperative outcome. Autosite mortality occurred in 15 (31%) of these cases. Cardiorespiratory failure associated with congenital cardiac defects in autosites was the most commonly cited cause of death [5–8]. Sepsis was also a major cause of mortality [4, 6, 9]. In one of these cases, autopsy revealed pneumonia [6].
CONCLUSION
Heteropagus autosite mortality is high as mentioned, so we do recommend early separation and emphasize wound closure with interrupted sutures as wound infection is common.
CONFLICT OF INTEREST STATEMENT
None declared.



