-
PDF
- Split View
-
Views
-
Cite
Cite
Yasir Mahnashi, Atheer S Alotaibi, Mohammad Aldakhail, Amer Alshahrani, Desmoid tumor at the gastrointestinal anastomosis after a one-anastomosis gastric bypass (mini-gastric bypass): a case report, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz411, https://doi.org/10.1093/jscr/rjz411
Close - Share Icon Share
Abstract
Desmoid tumors of the small bowel wall are rare tumors of the gastrointestinal tract. The signs and symptoms ranging from non-specific to severe abdominal pain to the sensation of a mass and abdominal fullness. We present the case of a 48-year-old man who presented 3 years post-one-anastomosis gastric bypass (mini-gastric bypass) with vague abdominal pain and early satiety of one-month duration. A CT scan of the abdomen revealed a well-defined compressive mass in the left hypochondrium. A laparoscopic exploration was performed, but it was converted into a laparotomy due to the huge size of the mass. The desmoid tumor at the gastrojejunal anastomosis was resected, followed by a Roux-en-Y reconstruction. The patient’s postoperative course was uneventful, and he was discharged on the seventh day post-operation. He did not show any signs or symptoms suggestive of complications or recurrence during his follow-up.
INTRODUCTION
A desmoid tumor is a type of fibromatosis, which is a benign proliferation of facial or musculoaponeurotic structures [1]. This tumor has a low tendency to metastasize, but it has the potential to invade local tissues. It can be superficial, arising from the shoulder, thigh, buttock or trunk, or it can be deep-seated, arising from the mesentery, especially from the small bowel. According to previous reports, intra-abdominal desmoid tumors occur in about 75% of patients with FAP, with 75% of them arising in the mesentery [1, 2].
We present a case of an intra-abdominal desmoid tumor arising from the small bowel following a mini-gastric bypass in a patient presenting with vague abdominal pain.
CASE REPORT
The patient was a 48-year-old male who presented to the emergency department (ED) with abdominal pain and discomfort of 1 month duration. The pain was mainly in the epigastrium and left hypochondrium and was described by the patient as a dull intermittent pain with a severity of 3 out of 10. The pain was not radiating and was not associated with aggravating or relieving factors. The patient also reported early satiety but no nausea, vomiting or constipation.
The patient denied any history of fever or unintentional weight loss. His surgical history was remarkable for a mini-gastric bypass that was performed 3 years ago. He had an initial body mass index (BMI) of 40 kg/m2 before the intervention; his BMI was lower (29 kg/m2) when he presented to the ED. The patient was a known case of hypertension and diabetes mellitus type 2 and was eventually taken off antihypertensive and hypoglycemic medication after the mini-gastric bypass. He had no family history of cancer.
During the physical examination, the patient’s vital signs were stable: temperature of 36.9 °C, heart rate of 62 beats per minute and oxygen saturation of 100% room air. Upon abdominal examination, a large, palpable, mobile, non-pulsatile, non-tender mass was found in the left upper quadrant. A digital rectal examination was not remarkable.
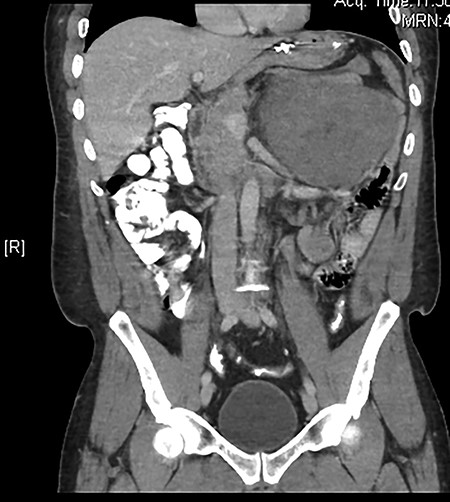
The results of routine blood investigations were within normal limits and an abdominal X-ray showed a normal bowel gas pattern. An abdominal computed tomography (CT) scan showed a huge, well-defined, inhomogeneous mass at the left hypochondrium measuring about 15.8 × 14.6 × 12.8 cm (Fig. 1). No signs of bowel distension or obstruction were observed. Magnetic resonance imaging showed that the mass and liver were metastasis-free. An esophagogastroduodenoscopy revealed a 1-cm smooth lesion in the mid-esophagus, which was positive for desmin and negative for CD117, with smooth muscle differentiation (most likely a leiomyoma). A colonoscopy revealed two hyperplastic rectosigmoid polyps, which were negative for malignancy or dysplasia. A provisional diagnosis was made for gastrointestinal stromal tumor.
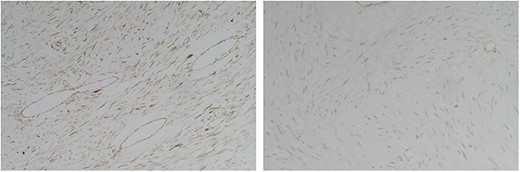
Immunohistochemical staining of the tumor cells showed positive nuclear staining for beta-catinine (A) and negative staining for CD117, DOG-1, SMA, CD34, and S100 (B) consistent with a desmoid tumor.
A laparoscopic exploration was performed; however, it was converted into a laparotomy with midline incision due to the large size and unclear nature of the mass. A large mass arising from the jejunal wall with a highly vascular smooth surface and a well-defined margin was observed at the gastrojejunostomy anastomosis (Fig. 2). The mass had a large feeding arterial supply arising from the mesentery of the small bowel. Another mass measuring 5 cm was found distal to the gastrojejunostomy. Surgical resection was performed with adequate proximal and distal resection margins, and the gastrojejunal anastomosis was disconnected from the distal stomach pouch. A Roux-en-Y gastric bypass was done. The patient’s post-operative course was uneventful, and he was discharged on the seventh day post-operation. He showed no complication or recurrence during his follow-up.

A computed tomography (CT) scan showed a well-defined, inhomogeneous mass at the left hypochondrium displacing the stomach, colon, and nearby organs.
A histopathology examination of both tumors revealed a desmoid-type fibromatosis arising from the small bowel. Nineteen lymph nodes were negative. Additionally, the resection margins were negative. Immunohistochemistry of the tumor cells showed positive nuclear staining for beta-catenin but negative staining for CD117, DOG-1, SMA, CD34, S100 and desmin consistent with the diagnosis of a desmoid tumor (Fig. 3).
Gross appearance of the resected mass arising from the jejunal wall.
DISCUSSION
Primary desmoid tumors are rare and contribute to 0.03% of all neoplasms and account for <3% of all soft tissue neoplasms [3]. These tumors are classified as extra- or intra-abdominal and can be found in the abdominal wall, with 50% occurring in the retroperitoneum, 9% in the mesentery and 40% arising from the small bowel wall [4]. The sporadic form of desmoid tumors is usually associated with abdominal surgery, pregnancy, hormone therapy and Gardner’s syndrome. Conversely, intra-abdominal desmoid tumors are rare and associated with FAP [1].
The patient in our case had a desmoid tumor arising from a gastrojejunal anastomosis after a mini-gastric bypass. To the best of our knowledge, only one case of a desmoid tumor after Roux-en-Y gastric bypass has been reported [2], but there is no report of this tumor after a mini-gastric bypass.
Patients with desmoid tumors typically present varying signs and symptoms, ranging from non-specific pain and discomfort to obstructive and pressure symptoms [2, 5–7]. The diagnosis is typically established based on a histopathology examination because the tumor may mimic other tumors, both grossly and radiologically [8].
Desmoid tumors usually have a well-circumscribed wall and an adjacent infiltrating structure, and immunohistochemistry is usually negative for CD117, DOG1, ALK1, S100, CD34, desmin and actin; positive for vimentin and beta-catenin [4].
Several treatment modalities, including targeted radiotherapy, hormone therapy, non-steroidal anti-inflammatory drugs and observation, have been proposed for intra-abdominal desmoid tumors [3], and these treatment options vary depending on the involvement of vital structures. Surgical resection with negative margins is still considered the treatment of choice for operable desmoid tumors [1], and it can decrease the recurrence rate by 25–50% [9].
Overall, a desmoid tumor of the small intestine wall is an unusual finding after a gastric bypass. The presentation is variable, and a diagnosis may be challenging before a histopathological examination. Although a desmoid tumor is considered benign, it has an increased potential for local invasion. Early presentation of the patient as well as early diagnosis and surgery, when feasible, can decrease the recurrence rate.
References



