-
PDF
- Split View
-
Views
-
Cite
Cite
Julian J L Leow, Cicatricial ectropion after wound closure of facial laceration, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz387, https://doi.org/10.1093/jscr/rjz387
Close - Share Icon Share
Abstract
Patients presenting to the emergency department with facial lacerations are commonplace and often sutured by a junior trainee. Cicatricial ectropion can occur after trauma, surgery and actinic/other dermatological conditions. It can make the eye dry, irritated and vulnerable to infection and water excessively. A 71-year-old man presented to the emergency department after falling off his bike. He had lacerations on his right forehead and right lower eyelid, amongst other injuries. His lacerations were sutured in the emergency department but 2 months later, he presented with scar contracture and was diagnosed with cicatricial ectropion of lower eyelid. This case highlights the risk of ectropion after closure of lacerations which involve the eyelid. Ectropion and how to reduce the risk involved surgically are discussed in this case report. Both diagnosing and operating clinicians should be aware of these risks and inform the patient appropriately.
INTRODUCTION
Ectropion can be classified into involutional, paralytic, mechanical, congenital and cicatricial ectropion. Cicatricial ectropion describes the turning of the eyelid outwards most often due to shortening of the anterior lamella comprising of the orbicularis muscle and skin. Other than the cosmetic deformity, it can make the eye dry, irritated and vulnerable to infection and cause the conjunctiva to keratinize [1]. In rare instances, it can cause blindness. Patients presenting to the emergency department with facial lacerations are commonplace and often sutured by a junior trainee. There are many factors that influence the risk of ectropion when closing lacerations involving the eyelid and it is important that both the clinician and the patient are aware of these factors.
CASE REPORT
A 71-year-old man presented to the emergency department after falling off his bike. He was diagnosed with a head injury, nasal fracture and lacerations on his right forehead and right lower eyelid. The head injury and nasal fracture were managed conservatively. Due to his right pupil being unreactive and rapidly declining vision, an emergency canthotomy and cantholysis was performed. His lacerations were sutured, and he had weekly follow-ups for 3 weeks with ophthalmology department. About 2 months later, the patient presented with scar contracture and outward rotation of his right lower eyelid. This was diagnosed as cicatricial ectropion (Figs 1 and 2). This was treated with scar revision, canthopexy and upper to lower lid switch flap (Figs 3 and 4). The patient was evidently anxious as his left eye was already blind from a previous ocular injury.
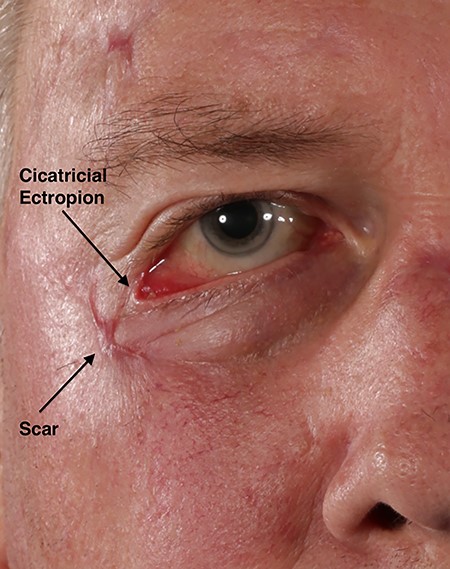
A 2-month old scar involving the lower eyelid of the right eye causing cicatricial ectropion.
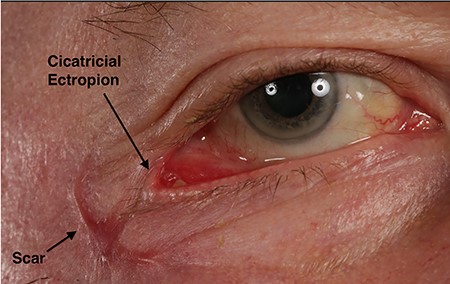
Close-up of a 2-month old scar involving the lower eyelid of the right eye causing cicatricial ectropion.


DISCUSSION
The posterior surface of the eyelid normally opposes the ocular surface. For the lower eyelid, the position of the eyelid is dependent on the physiological stability of the anterior lamella, posterior lamella and medial and lateral canthal ligaments. The anterior lamella consists of the skin and orbicularis muscle and the posterior lamella consists of the tarsus and conjunctiva. Horizontal eyelid laxity, orbicularis oculi muscle weakness and shortage of skin all contribute to ectropion [2]. As one ages, the skin loses elasticity, orbicularis oculi muscle weakens and the medial and lateral canthal tendons become more lax, permitting the lower eyelid to migrate inferiorly. Ectropion is the outward rotation of the eyelid margin which can affect the upper and lower eyelid. Cicatricial ectropion can occur after trauma, surgery and actinic/other dermatological condition. The ideal laceration orientation is perpendicular to lower eyelid margin (Fig. 5), as it reduces unwanted tension which would cause ectropion [3]. Lacerations perpendicular to this ideal orientation increase the risk of ectropion as seen in this case (Fig. 2), and patients should be warned of this increased risk. Table 1 discusses strategies for reducing ectropion risk.
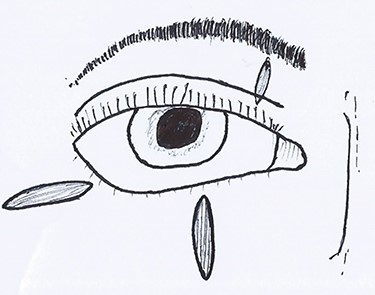
Ideal orientation of lacerations which have a lower risk of ectropion. Notice how the scar on this patient is perpendicular to the ideal.
| Strategies of reducing ectropion risk |
| • It is crucial to close the laceration in its layers. Importantly, the orbicularis muscle should be closed such that the skin is sutured together as tension-free as possible. |
| • Avoid suturing the laceration if it is already pulling on the eyelid. |
| • Undermine inferiorly to the laceration (away from palpebral fissure) to reduce tension. |
| • Place steristrips over the sutures if possible to reduce tension. |
| • Allowing the laceration to heal via secondary intention is usually not advisable due to the high incidence of cicatricial ectropion. |
| • Some lacerations should not be closed in the Emergency department where the lighting and equipment may not be ideal. |
| • Advice the patient to regularly massage their lower eye lid upwards after it has healed. |
| Strategies of reducing ectropion risk |
| • It is crucial to close the laceration in its layers. Importantly, the orbicularis muscle should be closed such that the skin is sutured together as tension-free as possible. |
| • Avoid suturing the laceration if it is already pulling on the eyelid. |
| • Undermine inferiorly to the laceration (away from palpebral fissure) to reduce tension. |
| • Place steristrips over the sutures if possible to reduce tension. |
| • Allowing the laceration to heal via secondary intention is usually not advisable due to the high incidence of cicatricial ectropion. |
| • Some lacerations should not be closed in the Emergency department where the lighting and equipment may not be ideal. |
| • Advice the patient to regularly massage their lower eye lid upwards after it has healed. |
| Strategies of reducing ectropion risk |
| • It is crucial to close the laceration in its layers. Importantly, the orbicularis muscle should be closed such that the skin is sutured together as tension-free as possible. |
| • Avoid suturing the laceration if it is already pulling on the eyelid. |
| • Undermine inferiorly to the laceration (away from palpebral fissure) to reduce tension. |
| • Place steristrips over the sutures if possible to reduce tension. |
| • Allowing the laceration to heal via secondary intention is usually not advisable due to the high incidence of cicatricial ectropion. |
| • Some lacerations should not be closed in the Emergency department where the lighting and equipment may not be ideal. |
| • Advice the patient to regularly massage their lower eye lid upwards after it has healed. |
| Strategies of reducing ectropion risk |
| • It is crucial to close the laceration in its layers. Importantly, the orbicularis muscle should be closed such that the skin is sutured together as tension-free as possible. |
| • Avoid suturing the laceration if it is already pulling on the eyelid. |
| • Undermine inferiorly to the laceration (away from palpebral fissure) to reduce tension. |
| • Place steristrips over the sutures if possible to reduce tension. |
| • Allowing the laceration to heal via secondary intention is usually not advisable due to the high incidence of cicatricial ectropion. |
| • Some lacerations should not be closed in the Emergency department where the lighting and equipment may not be ideal. |
| • Advice the patient to regularly massage their lower eye lid upwards after it has healed. |
CONCLUSION
This case highlights the risk of ectropion after closure of lacerations which involve the eyelid. Skin loss, age and orientation of laceration increase the risks. Patients should be warned of these risks prior to closure.
Sources of Support
None.
ACKNOWLEDGEMENTS
No other contributors.
Footnotes
†This paper was presented as a poster at the Royal Society of Medicine national conference: Beyond our shore: Humanitarian and Global maxillofacial surgery.



