-
PDF
- Split View
-
Views
-
Cite
Cite
Eduardo Ventura, Sílvia Dionísio, Ângela Ferreira, Rute Saleiro, Hugo Marques, Manuel Magalhães, Carlos Monteiro, Maxillary mesenchymal chondrosarcoma leading to a diagnosis of Li-Fraumeni syndrome, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz386, https://doi.org/10.1093/jscr/rjz386
Close - Share Icon Share
Abstract
Mesenchymal chondrosarcoma (MCS) is a rare histological variant of chondrosarcoma, with aggressive behaviour. Due to the unique nature of this disease, management strategies are not well established. Li-Fraumeni syndrome (LFS) is a rare cancer predisposition syndrome with a wide tumour spectrum, associated with TP53 germline mutations. We report a case of MCS of the maxilla, treated with surgical excision and adjuvant chemotherapy, in a patient with a past medical history of choroid plexus papilloma and a family history of early age first-degree cervical uterine cancer, that led to the clinical suspicion of a cancer predisposition syndrome and the subsequent diagnosis of LFS. This is the first MCS described in a LFS case. It demonstrates that adjuvant chemotherapy should be considered, in conjunction with surgical excision, in MCS and that cancer predisposition syndromes should be suspected in patients with multiple neoplasms and a strong family history of cancer.
INTRODUCTION
Mesenchymal chondrosarcoma (MCS) is a rare histological variant of chondrosarcoma that is mostly seen in young adults, unlike conventional chondrosarcomas. It usually presents aggressive behaviour with an inclination for late recurrence and metastasis. Due to the rare nature of this disease, management strategies are not well established, but extensive surgical resection is unanimously described as the mainstay of treatment [1]. Nevertheless, due to the scarcity of clinical cases and data in the literature, the effectiveness of adjuvant chemotherapy and radiotherapy in addition to an ablation strategy is not well defined.
Li-Fraumeni syndrome (LFS) is an aggressive cancer predisposition syndrome, with a broad tumour spectrum, associated with TP53 germline mutations. The neoplasms reported most often are soft tissue sarcomas, osteosarcoma, premenopausal breast cancer, brain tumours and adrenocortical carcinomas [2].
CASE REPORT
A 35-year-old male patient was referred to our department, complaining of a painless, rapid growing exophytic gingival mass in the maxilla with two months’ duration. He had a previous history of choroid plexus papilloma, treated with surgery and radiosurgery at the age of 23. His mother was diagnosed with cervical uterine cancer at the age of 38.
On examination, a lobulated, firm mass was seen extruding from the anterior maxillary vestibule (Fig. 1). All maxillary teeth were painless to percussion, and normal tooth mobility was present. No cervical lymphadenopathy was detected, nor any changes with cranial nerve examination. A maxillofacial computerized tomographic (CT) scan revealed an osteolytic lesion on the maxillary alveolar process (Fig. 2).

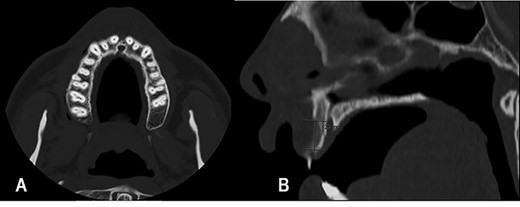
Maxillofacial CT scan, axial (A) and sagittal (B) images. Osteolytic lesion on the vestibular edge of the maxillary alveolar process, with 12 mm of craniocaudal dimension and 4 mm of axial dimension.
We performed an incisional biopsy of the mass that revealed findings suggestive of a preliminary diagnosis of MCS. After discussion in a multidisciplinary Head and Neck Oncology meeting, the team decided that surgery and adjuvant chemotherapy was the most appropriate treatment plan.
Surgical access was obtained intraorally, and an en bloc resection of the premaxilla was performed (Fig. 3). Histopathological examination confirmed the diagnosis, revealing a completely resected MCS with clear margins (Fig. 4).
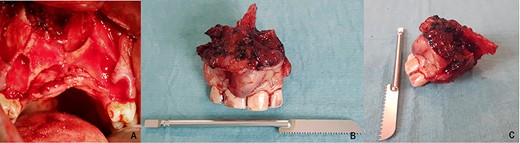
After en-bloc resection of the premaxilla (A). Frontal (B) and lateral (C) view of the surgical specimen.
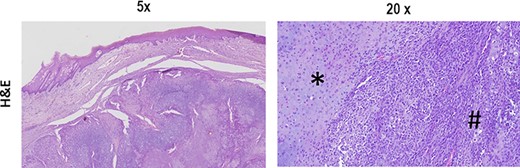
The typical biphasic pattern of MCS, composed of islands of cartilage (*) admixed with poorly differentiated small round cells with scant cytoplasm (#). H&E stain.
The patient underwent an adjuvant chemotherapy regimen with vincristine, doxorubicin, cyclophosphamide/ifosfamide and etoposide (VAC/IE), completing 12 cycles uneventfully. He was referred to the Medical Genetics Department, where further studies confirmed a pathologic variant on the TP53 gene and the diagnosis of LFS.
With 34 months of follow-up, the patient is asymptomatic without any local signs of recurrence, and a good functional and aesthetical result was accomplished with a removable partial denture (Fig. 5). At present, he is in a strict cancer surveillance regimen based on the NCCN protocol.

Rehabilitation with a removable partial denture (A). Frontal view after oral rehabilitation (B).
DISCUSSION
MCS is a rare histological variant of chondrosarcoma, mostly seen in young adults, unlike conventional chondrosarcoma that shows a propensity for older age groups. When present in the head and neck area, this condition shows a predisposition for the maxillary anterior alveolus, due to the presence of nasal cartilage [1].
A study of 36 MCS of the maxilla demonstrated that the most common clinical presentation was a mass or growth in 68% of cases, followed by nasal obstruction (32%), epistaxis (32%) and tooth mobility (24%) [3]. In our report, the patient’s chief complaint was a rapid protruding mass that possibly due to its exophytic nature was not associated with nasal symptoms or tooth mobility.
Diagnosis of MCS can only be established by histopathological examination, characterized by a biphasic pattern, with a sheet-like or patternless proliferation of small differentiated spindle or round cells surrounding discrete nodules of differentiated hyaline cartilage [3].
Extensive surgical resection is described unanimously as the mainstay of treatment but, due to the scarcity of clinical cases and data in the literature, the effectiveness of adjuvant chemotherapy and radiotherapy is not well defined, and consensus has not been reached on the optimal management of MCS [1]. In this case report, the patient received a VAC/IE Adjuvant Chemotherapy scheme, in compliance with the NCCN Clinical Practice Guidelines [4] with excellent tolerability and minimal side effects.
MCS presents aggressive behaviour, with a tendency towards local and distant recurrences, which can occur as late as 20 years following diagnosis, making long-term follow-up extremely important [5]. The overall prognosis is poorer than with conventional chondrosarcomas, with reported 10-year survival rates ranging from 10 to 28% [1, 5].
LFS is one of the most aggressive cancer predisposition syndromes described. It is an autosomal dominantly inherited condition caused by germline mutations of TP53 suppressor gene encoding p53 [2]. Classically, it has been diagnosed with the use of the Chompret criteria [6] to identify patients who warrant genetic testing for the presence of pathologic variants of germline TP53 [7]. The tumour spectrum of LFS is broad, but the neoplasms reported most often are soft tissue sarcomas, osteosarcoma, premenopausal breast cancer, brain tumours and adrenocortical carcinomas [2]. One hospital-based analysis revealed that the lifetime cancer risk of TP53 gene mutation carriers was estimated to be 73% in males and nearly 100% in females, with the high risk of breast cancer accounting for the difference [8, 9]. Since TP53 mutation carriers enrolled in a surveillance program have improved survival, early diagnosis is a critical matter, and these patients should be followed according to one of the surveillance protocols already published [2].
In our case, the rare nature of MCS, the history of choroid plexus papilloma and the history of the patient’s mother developing uterine cancer at the age of 38 lead us to the suspicion of a cancer predisposition syndrome that was confirmed by our Medical Genetics Department.
In conclusion, to the best of our knowledge, this is the first MCS described in a LFS case. Cancer predisposition syndromes should be suspected in patients with multiple neoplasms and a strong family history of cancer because surveillance protocols improve survival. A QT scheme with VAC/IE should be considered in conjunction with surgical excision in MCS cases. Long-term follow-up is imperative due to the high frequency of late local or distant recurrences.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Susan Foreid and Dr Macedo Dias, who kindly provided the histopathological images and Dr Carlos Miranda for granting us the initial presentation picture.
CONFLICT OF INTEREST STATEMENT
We have no conflicts of interest.



