-
PDF
- Split View
-
Views
-
Cite
Cite
Darius Khadembaschi, John Arvier, Nicholas Beech, David Dolan, Jim McGill, Successful management of severe coronoid process hyperplasia in a patient with mucopolysaccharidosis VI: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz388, https://doi.org/10.1093/jscr/rjz388
Close - Share Icon Share
Abstract
Mucopolysaccharidoses are a group of rare lysosomal storage diseases caused by a deficiency of enzymes, which breakdown glycosaminoglycans, with consequent dysfunction of affected tissues. Mandibular coronoid hyperplasia, with associated trismus, has been recently described as a feature of the craniofacial abnormalities seen in these patients. However, the details of the surgical and post-operative management of these patients have not been previously documented. This case describes the successful management of severe trismus from coronoid process hyperplasia in a 14-year-old male, utilising an extra-oral approach for bilateral coronoidectomies and removal of exophytic zygomatic bone, followed by immediate and long-term physiotherapy. An improvement of mandibular opening from 8 to 45 mm has been maintained at 18 months post operation.
INTRODUCTION
Mucopolysaccharidoses (MPS) are rare (1 in 25 000) lysosomal storage diseases due to a deficiency of enzymes involved in degradation of glycosaminoglycans (GAGs) and are classified into seven clinical sub-types [1, 2].
The features of MPS arise from the intracellular and extracellular accumulation of unprocessed or partly processed GAGs in lysosomes and progressive dysfunction of affected tissues [2]. Features include organomegaly; abnormal facies, including flat nasal bridge and thick lips; impaired vision; hearing loss; cardiovascular dysfunction; progressive neurological decline in some types (not MPS type VI); restricted joint mobility and skeletal abnormalities [1, 3].
The craniofacial features of MPS include a thickened calvarium, macrocephaly, a lack of pneumatization of the mastoid process and paranasal sinuses, and a short and broad mandible with an underdeveloped mandibular condyle [2]. Coronoid process hyperplasia (CPH) has also been recently described as a feature of MPS, and in cases of severe trismus, coronoidectomy may be required to increase mouth opening [4].

Preoperative maximal inter-incisal distance, approximately 8 mm.

Preoperative CT ((A and D) axial sections, (B) coronal section, (C) 3D reconstruction) demonstrating CPH (red arrows), concavity of the ramus (stars) and bony deposits on the medial aspect of zygomatic arches (blue arrows).
CASE REPORT
A 14-year-old male with severe MPS VI was referred due to a progressive reduction in mouth opening. The trismus was first noticed at laryngoscopy 2 years previously, and subsequent intubations for ophthalmic surgery had become increasingly difficult. Although he presented with typical MPS morphology, he was less affected than his older sibling, a difference attributed to treatment with enzyme replacement therapy from 8 weeks of age [5].
On examination, the patient’s maximal inter-incisal distance was only 8 mm (Fig. 1). A CT scan confirmed marked coronoid hyperplasia bilaterally, and the thickened anterior borders of the rami created concave surfaces on the superolateral aspect of the mandible (Fig. 2A). The condyles appeared hypoplastic although otherwise fully functional and non-ankylosed, and the superior aspect of the coronoid processes deviated laterally, curving over the superior aspect of the zygomatic arch on both sides. (Fig. 2B and C). In addition, exophytic bone deposits had formed on the medial aspect of the zygomatic arches suggestive of either benign exostosis or reactive hyperplasia (Fig. 2D).
The indications for surgery included difficulties with daily activities, as well as the projected likelihood of regular intubations and further surgery in the near future. The patient subsequently underwent bilateral coronoidectomies and removal of the zygomatic arch exostoses under general anaesthesia. Due to the predicted difficulty with direct laryngoscopy, a fibre-optic technique was used. Due to the young age of the patient, anaesthesia was induced by a mask, and a fibre-optic bronchoscope was placed through the nose and positioned in the trachea. An endotracheal tube was then guided over the bronchoscope, and the subsequent general anaesthesia was uneventful.
As expected, the lateral concavity of the mandible limited intra-oral access to the sigmoid notches, and a bicoronal flap was raised. Osteotomy and lateral reflection of the right zygomatic arch were required for access to divide the temporalis and complete the coronoidectomy on that side. A partial improvement in mouth opening resulted, facilitating easier coronoidectomy and removal of the exophytic bone without arch division on the left side (Fig. 3A). The mandible was vigorously mobilised, and an intraoperative mouth opening of 40 mm was achieved (Fig. 3B).
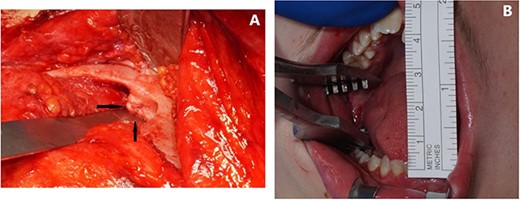
Intraoperative. (A) Superior view of left zygomatic arch, demonstrating exophytic bone on the anteromedial surface. (B) Mouth opening 40 mm.
The patient was transferred to ICU for recovery, with the endotracheal tube left in overnight. The bite block was maintained in situ for 48 hours to stretch local soft tissues and encourage cognitive awareness of the expected range of mandibular movement. The patient subsequently made uneventful progress. At Day 7, the scalp sutures and staples were removed under general anaesthesia, and the bite block was reinserted for a further 48 hours.
Postoperative physiotherapy commenced immediately after removal of the bite block, utilising a TheraBite® at maximal opening for 3 minutes, before meals. Excellent mouth opening has been maintained over the follow-up period with unassisted inter-incisal measurement of 45 mm, and assisted opening of 50+ mm, at 18 months post operation (Fig. 4).
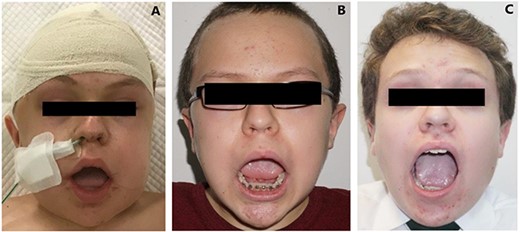
Postoperative progress. (A) Immediately post-op with bite block in situ. (B) 4 weeks post-op. (C) 18 months post-op.
Histopathology of the zygomatic exostoses showed essentially normal cortico-cancellous bone, with small amounts of additional fibro-cartilage, and the aetiology remains uncertain.
DISCUSSION
MPS is a rare condition with widespread systemic complications. A recent study on 80 MPS patients described 61 with limited mouth opening below the 10th percentile [4]. Five of the most severely affected patients (mouth opening <25 mm) underwent bilateral coronoidectomy with postoperative physiotherapy. An average of 10 mm increase in interincisal measurement was achieved at 12 months post-operation [4].
CPH may also occur in the general population, although no epidemiological studies have been conducted [6]. Suggested aetiological factors include temporalis muscle hyperactivity, mandibular hypomobility, and local trauma [6]. In cases of MPS, the CPH may be associated with generalised skeletal changes caused by the effects of GAGs deposition, which is known to alter osteoclast morphology and function in animal models [7, 8].
Intraoral and extraoral approaches for coronoidectomy and coronoidotomy have all been described [6, 9]. Simple sectioning of the coronoid has been successful in some cases, and although there is less local morbidity, coronoid reattachment may occur [6]. In the presented case, full coronoidectomy was preferred due to the patient’s obvious propensity for exuberant bone formation. An extraoral approach was required for adequate access to divide temporalis and facilitate coronoid resection.
Post-operative physiotherapy in considered a key factor in maintaining mouth opening [6, 10]. We have found retaining the bite block in situ post-operatively to be particularly efficacious. This may cause initial apprehension in parents and nursing staff. However, pre-operative reassurance generally alleviates their concerns. Longer term physiotherapy with the TheraBite®, reinforced by diligent parental supervision, has maintained the good improvement in the range of mandibular movement in this case. We have found this post-operative protocol very helpful in managing a variety of surgical cases with limited mouth opening and impaired TMJ function.
This case report demonstrates successful management of severe CPH in a patient with MPS. An extraoral approach provided adequate access for bilateral coronoidectomy and removal of exophytic zygomatic bone. Post-operative physiotherapy appears to have maintained the significant increase in mouth opening at 18 months post-operatively. The improvement in function has been profound, and the likelihood of relapse now seems remote.
References
Mucopolysaccharidoses Fact Sheet. National Institute of Neurological Disorders and Stroke Bethesda, MD 20892: Office of Communications and Public Liaison. National Institutes of Health, 2019. https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/mucopolysaccharidoses-fact-sheet.



