-
PDF
- Split View
-
Views
-
Cite
Cite
Edmund Wooi Keat Tan, Jason Bae Barco, Mutee Ur Rehman, Choon Chieh Tan, Retromastoid osteoma—a rare case report, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz381, https://doi.org/10.1093/jscr/rjz381
Close - Share Icon Share
Abstract
Osteomas are slow growing bone tumours and are often asymptomatic. Rarely, they can be present in the temporal bone—only few cases had been reported, with an incidence of 0.1–1%. We describe a case of an osteoma of the temporal bone (retromastoid) found in a 40 year old female, who presented with a slow growing swelling behind the right ear for 9 years. Diagnosis was made on non-contrast computed topography (CT) of the skull. Treatment is indicated in symptomatic cases or cosmetic reasons. Screening colonoscopy and genetic testing for familial adenomatous polyposis (FAP) and Gardner’s syndrome are advised.
INTRODUCTION
Osteomas are benign bone tumours. They are mostly asymptomatic and slow growing. Only a handful of cases were reported on temporal osteomas, with an incidence of 0.1–1% [1].
Osteomas can be subdivided based on location, more commonly sino-orbital (or paranasal sinus) osteomas and bone surface tumours (or exostoses) that arise from the cranial vault, mandible or the external auditory canal [2, 3]. Osteomas arising from the outer table larger than 3 cm are considered to be giant tumours [4, 5]. Most osteomas are asymptomatic and have a tendency to grow slowly. The clinical presentation would based on location, size and extension of the tumour.
CASE REPORT
A 40 year-old female presented to the outpatient department with the primary complaints of a hard swelling over the post-auricular region for 9 years which had slowly increased in size.
She felt the sensation of protrusion and pressure upon lying on the right side of her head when she sleeps, otherwise, no complaints of pain or other associated symptoms related to the swelling.
There was no history of any previous injury or infection to the area. No family history of such lumps.
On examination, there is a solitary bony hard 2 cm × 2 cm swelling over at the right post-auricular region. Covered and surrounded with healthy skin, no overlying skin changes, ulceration, erythema or punctum was seen. It is not mobile, fixed to the underlying bone and non-tender.
X-ray skull AP & lateral views (Fig. 1) did not show bony erosions, lytic lesions or sclerotic lesions which if present would indicate a possible infectious, inflammatory or neoplastic process. However, the bony swelling was difficult to assess on X-ray due to orientation.
Non-contrast CT scan of the skull (Fig. 2) reported an outer table right retromastoid exophytic osseous mass, measuring 1.7 cm at its base. No destructive skull lesion and no intracranial extension were reported.
The provisional diagnosis of a retromastoid osteoma was made.
Based on the presenting complaint, main indication of surgical resection would be of cosmetic alteration in this case.
She was counselled accordingly and opted for conservative management for the temporal osteoma. Screening for Gardner’s syndrome was negative.
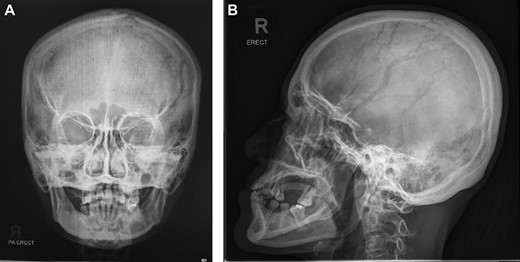
A relatively normal X-ray skull which did not show any significant pathology.
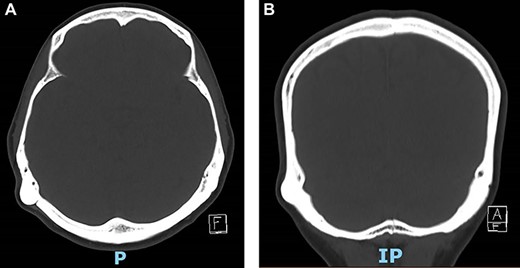
Computed tomography (CT) of temporal bone showing retro-mastoid osteoma in axial and coronal plane.
DISCUSSION
The pathogenesis of osteomas is controersial. Three main theories were identified, namely embryologic, infectious or traumatic. [7].
They can also be further subdivided based on the proportions of dense and cancellous bone; [6] non-contrast CT scan is the imaging of choice.
Ivory osteomas composed of dense, mature, lamellar bone with little fibrous stroma; on imaging, they appear to have similar radiodenstiy to normal cortex.
Mature osteomas composed of large trabecular of mature, lamellare bone with more abundant fibrous stroma with or without osteoblastic rimming, demonstrate central marrow, appearing as well-demarcated, radiodense opacity with dense growth of sclerotic lesion on imaging.
Mixed type have both features of ivory and mature osteomas.
The treatment options include en bloc resection or grinding of the tumour using high-speed drill. Surgical resection is mainly performed in symptomatic cases with constant pain, neurological symptoms and extension to adjacent structure or cosmetic alterations. Craniotomy with cranioplasty may be considered for giant tumours.
In addition, the management of young patients with cranial osteomas would require a screening colonoscopy or genetic testing for FAP or Gardner’s syndrome. Up to 24% of patients with FAP or Gardner’s syndrome are associated the development of craniofacial osteomas [1]. Though benign osteomas are harmless in most cases, these patients have a high risk of developing gastrointestinal malignancy at a young age.
ACKNOWLEDGEMENTS
The authors of this article are grateful towards the members of Sengkang General Hospital, Singapore without whose support and facilities, writing of this article would not be possible.
CONFLICT OF INTEREST
Upon the completion of this article, there are no conflicts of interest to declare.



