-
PDF
- Split View
-
Views
-
Cite
Cite
Hong L Lee, Rhonda Farrell, Vasanth Kamath, Ivan Ho-Shon, Francis Yap, Concordant PET/CT and ICG positive lymph nodes in endometrial cancer: a case of mistaken identity, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz377, https://doi.org/10.1093/jscr/rjz377
Close - Share Icon Share
Abstract
Endometrial carcinoma is the most common gynecological malignancy in developed countries. In early stage endometrial cancer, routine systemic pelvic lymphadenectomy showed no survival benefits and results in increased morbidity. The role of PET/CT imaging for the pre-operative detection of lymph node metastases in endometrial cancer is unclear. Sentinel lymph node (SLN) mapping may reduce the surgical staging morbidity while maintaining prognostic information of the lymph node status. Recently, indocyanine green (ICG) SLN mapping has been utilized to detect nodal metastasis in endometrial cancer. Endosalpingiosis is defined as the presence of tubal-like epithelium outside of the fallopian tube and can sometimes be misinterpreted as cancer metastasis. Here, we discuss a patient with newly diagnosed endometrial cancer who had pelvic and para-aortic lymph nodes with high glucose avidity on PET/CT, and ICG positivity on SLN mapping, suspected clinically to be metastatic adenocarcinoma, but with the pathological finding of endosalpingiosis only.
INTRODUCTION
Endometrial carcinoma is the most common gynecological malignancy in developed countries with an incidence of 14.7 per 100 000 [1]. Lymph node metastasis is one of the most important prognostic factors, as reflected in the current FIGO staging system [2].
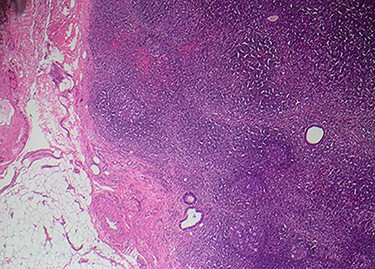
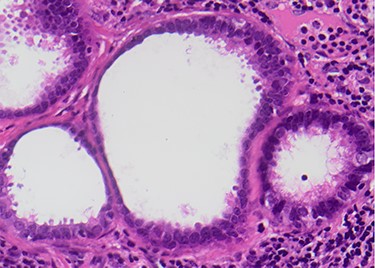
Endosalpingiosis is defined as the presence of tubal-like epithelium outside of the fallopian tube (Figs 1 and 2) [3]. The occurrence of endosalpingiosis can sometimes be misinterpreted as adenocarcinoma metastasis [4].
We discuss a patient with newly diagnosed endometrial cancer with pelvic and para-aortic lymph nodes which demonstrated high glucose avidity on PET/CT, and indocyanine green (ICG) positivity on sentinel lymph node (SLN) mapping, suspected clinically to be metastatic adenocarcinoma, but with the pathological finding of endosalpingiosis only.
CASE REPORT
A 47-year-old premenopausal woman, presented with a 3 month history of irregular vaginal bleeding. Ultrasonography revealed an endometrial thickness of 31 mm. Hysteroscopy, dilation and curettage was performed. Histology revealed Grade 1 endometrioid endometrial carcinoma. A CT scan of the chest, abdomen and pelvis was performed and demonstrated a 9.9-mm ground glass nodule in the upper lobe of the right lung. Histology of the nodule revealed adenocarcinoma arranged in a lepidic pattern with an immunoprofile consistent with primary lung cancer. An FDG-PET/CT was performed (Fig. 3), and there was intense FDG uptake in the uterus corresponding to the primary tumor. Moderate to intense FDG accumulation was also seen corresponding to a tubular mass located posteriorly to the uterus, thought to represent the fallopian tube and ovary. There was further moderate FDG accumulation in a right external iliac lymph node and in an aortocaval lymph node at the level of the right renal hilum (Fig. 3) located behind the duodenum, and very mild FDG accumulation corresponding to an ill-defined ground-glass opacity in the upper lobe of the right lung laterally.
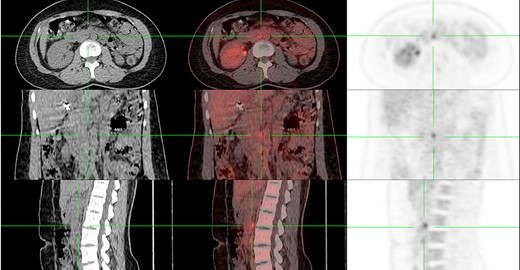
FDG avid aortocaval lymph node at the level of the right renal hilum (7 mm in short axis, SUVmax 5.9) on PET/CT
After multidisciplinary discussion, gynecological surgery was planned first due to the low-grade nature of the lung cancer and acute vaginal bleeding symptoms. Because of the location of the high para-aortic lymph node, the patient underwent laparotomy rather than a laparoscopic approach. After discussion, the patient did not agree to a complete lymph node dissection due to concerns around lymphoedema, and consented to the removal of any clinically suspicious lymph nodes at the time of surgery with SLN identification enhanced by ICG. Intra-operatively, two SLN sites were located and removed.
Final histology revealed Grade 1 endometrioid adenocarcinoma, confined to the uterine body, invading the myometrium 10 mm through a wall 26-mm thick. No evidence of lymphovascular invasion was seen and the pelvic washings were negative. The right ovary contained a hemorrhagic corpus luteal cyst and the right fallopian tube showed features of an acute on chronic salpingitis and pyohydrosalpinx. The fallopian tubes and ovaries were benign. Both ICG-positive lymph nodes showed endosalpingiosis, which was CK7, ER and PAX8 immunopositive with an Ki67 proliferation index of less than 1%.
The patient’s diagnosis was stage 1A endometrial cancer with no further treatment indicated. She underwent excision of the lung lesion a few months later. Due to concerns around possible missed carcinoma in retained lymph nodes, PET/CT scan was repeated and was negative. There is no evidence of recurrence 18 months post-surgery.
DISCUSSION
We report a case of a premenopausal woman with synchronous endometrial and lung cancer, where endosalpingiosis, and not malignancy, was found in corresponding PET/CT-positive and sentinel ICG-detected pelvic and para-aortic lymph nodes. To the best of our knowledge, this is the first report where endosalpingiosis has mimicked malignancy on both pre- and intra-operative assessment of an endometrial cancer.
It is important to consider how endosalpingiosis might arise in the SLN basin in endometrial cancer. The nodal groups containing endosalpingiosis in our case are the same lymph node groups that endometrial carcinoma is reported to metastasize to and corresponds to the lymphatic drainage of the endometrium. The theory of lymphatic spread of tubal epithelium in a similar way to form nodal deposits of endosalpingiosis is plausible.
To explain why endosalpingiosis could result in high FDG-avidity on PET imaging, it is important to recognize that the accumulation of the radioactive glucose analog, FDG, is observed not only in malignancy but also in inflammatory cells [5]. In our case, there was concurrent salpingitis, which has been previously reported in association with nodal endosalpingiosis [6]. Kistner has described the theories of tubal reactivity and metastasis in the development of endosalpingiosis, which provides a novel explanation for why the endosalpingiotic lymph nodes were FDG avid—namely, that inflammation of the fallopian tube was likely to have occurred first, with lymphatic spreading of the inflamed tubal epithelium to the SLN groups following [6]. We can theorize that the endosalpingiotic ‘seeding’ of lymph nodes occurs in a chain reaction manner, and this is possibly what accounts for the fact that the lymph nodes moving further away from the initial inflamed fallopian tube was progressively less FDG avid. The possibility of ‘true positive’ PET/CT avid lymph nodes not being removed surgically, even with ICG localization, was ruled out by the negative repeat PET/CT 12 months post-operation without any adjuvant therapies.
This case highlights the real possibility of endosalpingiosis in lymph nodes causing ‘false positive’ PET scan findings in a patient with gynecological cancer. In our case, this finding led to incorrect clinical staging of endometrial cancer prior to definitive surgery, with the use of a more radical surgical approach to remove the PET/ICG positive para-aortic lymph node than would usually be undertaken. It is also possible that in some centers where PET/CT imaging is used pre-operatively to assist in staging, a similar patient may not have had surgical staging in the upper abdomen and may have been over-treated with adjuvant chemotherapy or radiation for a presumed stage 3C2 endometrial cancer. A multidisciplinary approach to the review of all pre-operative imaging used for clinical staging and matching these findings to the surgical pathology is paramount if we are to achieve the best outcomes for our patients with gynecological malignancy.



