-
PDF
- Split View
-
Views
-
Cite
Cite
Yujiro Yokoyama, Sarang Kashyap, Edward Ewing, Robert Bloch, Gastrosplenocolic fistula secondary to non-Hodgkin B-cell lymphoma, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz376, https://doi.org/10.1093/jscr/rjz376
Close - Share Icon Share
Abstract
Gastrocolic fistula (GSF) is a rare entity that arises mainly from splenic or gastric lymphoma. Gastric and splenic lymphomas can also fistulate with other organs, including the pleura and the colon, but there has been no reported case to best of our knowledge of a fistula involving three different organs. We hereby present the case of a female patient with gastrosplenocolic fistula secondary to non-Hodgkin B-cell lymphoma. We performed an en bloc partial gastrectomy with splenectomy and partial left colon resection with colostomy. GSF can be treated with chemotherapy. However, when the definite diagnosis is unclear or GSF is causing serious complications such as bleeding or active infection, we believe surgical excision is the treatment of choice.
INTRODUCTION
Gastrosplenic fistula (GSF) is a very rare and potentially fatal condition. GSF has not been adequately researched because of its rarity, but a recent systematic review of this condition reported that it mainly occurs in patients with lymphoma and most commonly managed with radical resection of involved organs [1]. We report a patient with gastrosplenocolic fistula secondary to non-Hodgkin B-cell lymphoma, which was successfully treated with surgical management.
CASE REPORT
A 63-year-old female presented to our hospital with a 2-week history of dark stools and coffee-ground emesis associated with anorexia, nausea, mild epigastric pain and shortness of breath. She denied fever or recent weight loss. Past medical history was significant for type II diabetes mellitus, hypothyroidism, hypertension and diverticulosis. She had no history of prior EGD. Her last colonoscopy was 5 years ago and colonoscopic resection of polyps was performed, which were precancerous. No significant surgical history. She is a nonsmoker and nonalcoholic. On presentation, the vital signs were unremarkable. Work up revealed white cell count of 31.3 × 103/μl and hemoglobin of 2.9 g/dl. The patient was admitted to the intensive care unit and
resuscitated with 4 units of packed red blood cell. Upper endoscopy was suspicious for a large paraesophageal hiatal hernia with necrotic mucosa and adherent clot versus penetrating proximal gastric ulcer (Fig. 1) as a possible source of upper gastrointestinal bleeding. Computed tomography showed a largeheterogeneous mass occupying the spleen with air suspicious for splenic abscess versus large mass perforating stomach and colon (Fig. 2). She underwent exploratory laparotomy, en bloc partial gastrectomy with splenectomy and partial left colon resection with colostomy. GSF was observed with the greater curvature of the stomach and a splenocolonic fistula was observed with the splenic flexure of the colon (Fig. 3). There was tumor
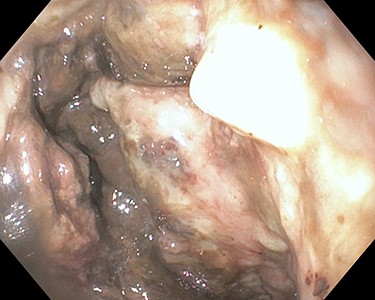
Esophagogastroduodenoscopy showing necrotic mucosa over the greater curvature of the stomach on retroflex view
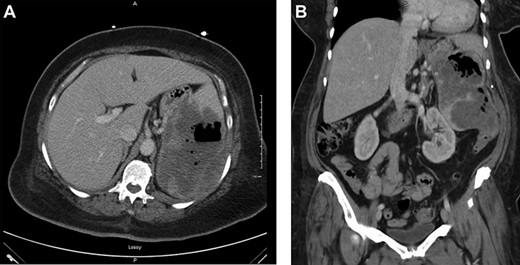
(a) Axial view of CT scan with intravenous contrast showed gastrocolic fistula. (b) Coronal view of contrast-enhanced abdominal CT scan. Large splenic mass fistulating into stomach and colon
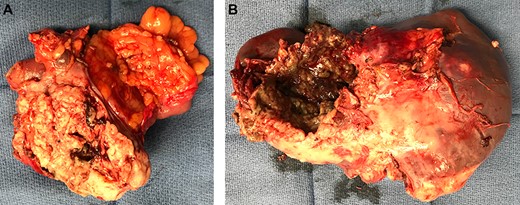
(a) Specimen showing gastrosplenocolic fistula. (b) Lateral side of spleen shows splenocolic fistula
invading the retroperitoneum and lateral abdominal wall, which was shaved off.
Her postoperative course was complicated with atrial fibrillation but she was eventually discharged home on postoperative day 9.
Fluorescence in situ hybridization target gene analysis was performed on the specimen. Aggressive non-Hodgkin diffuse large B-cell lymphoma (DLBCL) involving the spleen, the stomach and the colon with formation of gastrosplenocolic fistula and six uninvolved mesenteric lymph nodes were reported (Fig. 4). There was no evidence of BCL2/BCL6/MYC gene rearrangement.
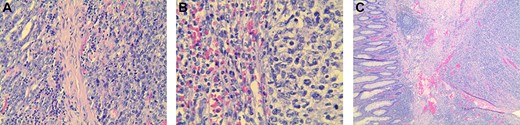
Histopathological slides showing specimen of stomach, spleen and colon. Atypical lymphoma cell were found in each organ specimen on hematoxylin–eosin stain. (a) Hematoxylin–eosin stain of the stomach specimen (benign tissue on the left and lymphoma on the right). (b) Hematoxylin–eosin stain of the spleen specimen (benign tissue on the left and lymphoma on the right). (c) Hematoxylin–eosin stain of the colon specimen
DISCUSSION
GSF is very rare and arises mainly from splenic or gastric lymphoma. The most common histopathological subtype is DLBCL [1]. Other etiologies include gastric adenocarcinomas, Crohn’s disease, benign gastric ulcers, post laparoscopic sleeve gastrectomy [2] GSF and trauma. Gastric and splenic lymphomas can also fistulate with other organs, including the pleura [3] and the colon [4]. Our literature review did not reveal any reported case of fistula involving three different organs. We believe this is the first case to be reported in literature.
GSF is known to occur in patients with splenic lymphomas either de novo or post-chemotherapy. Initial presentations of GSF are non-specific [5], such as weakness, fever and abdominal pain, so the diagnosis of GSF may be difficult and delayed. CT scan is the most useful tool, which can identify GSF-associated complications, such as abscess or bleeding, and can aid in the evaluation of the disease extent and surgical planning. Fluorodeoxyglucose (FDG) Positron emission tomography (PET)/Computed tomography (CT) has been reported to be useful in diagnosis of GSF [6].
Early diagnosis of GSF can be challenging. Delay in diagnosis leads to unfavorable outcomes. The presence of air in the spleen in patients with DLBCL should alert physicians to the possibility of GSF. The early diagnosis of spontaneous GSF without a known history of DLBCL is even more challenging. Therefore, radiologists, emergency room physicians, gastroenterologists and surgeons should be aware of this rare disease entity.
Radical surgical resection with splenectomy and partial gastrectomy is the most common treatment option. Although one laparoscopic case was reported [7], open approach seems common. The mainstay of treatment of DLBCL is chemotherapy with or without radiation [8]. Not all patients with GSF with DLBCL would require surgery. GSF without complications such as bleeding and perforation can be treated with chemotherapy alone without surgical intervention. Successful treatment of GSF with chemotherapy was reported recently [9]. When non-surgical treatment is chosen, tissue diagnosis with either endoscopic or percutaneous biopsy is required.
Splenocolonic fistula is also a rare condition. Etiology includes colon carcinoma involving the splenic flexure [10], primary cyst of the spleen and splenic hydatid cyst. There is no systematic review of this disease but successful treatment with left hemicolectomy with splenectomy is an option.
In our case, we did not have a definitive diagnosis, and considering her relatively young age and severe anemia, we believe surgical resection was appropriate at that time.
Conflict of interest statement
None declared.



