-
PDF
- Split View
-
Views
-
Cite
Cite
Iku Abe, Masaaki Saito, Taro Ikeda, Rintaro Fukuda, Akira Tanaka, Toshiki Rikiyama, Ileectomy performed on a case of adult intussusception due to inversion of Meckel’s diverticulum, Journal of Surgical Case Reports, Volume 2020, Issue 1, January 2020, rjz367, https://doi.org/10.1093/jscr/rjz367
Close - Share Icon Share
Abstract
We report a rare case of adult intussusception caused by an inverted Meckel’s diverticulum with ectopic pancreatic tissue. A 43-year-old woman was referred to our hospital with complaints of abdominal distention, intermittent abdominal pain and nausea that she experienced 3 months ago. Abdominal computed tomography scans demonstrated ileo-ileal intussusception that contained a tumor with fat density as the lead point. Laparoscopic-assisted partial resection of the small intestine was performed. The surgical specimen showed an elongated polypoid lesion invaginated into the intestinal tract indicating an inverted Meckel’s diverticulum. Pathological findings showed a true diverticulum that ran antimesentrically, with tall columnar epithelium, a mucous gland and an islet of Langerhans. The postoperative period was uneventful, and she was discharged on the ninth postoperative day.
INTRODUCTION
Among adult intussusception cases, those developing from Meckel’s diverticulum (MD) are relatively rare [1]. In particular, cases with ectopic pancreas in MD constitute only a small portion of the existing literature. Here, we report a case of intussusception from inverted MD with ectopic pancreas that was treated by laparoscopic surgery.
CASE REPORT
A 43-year-old woman presented with vomiting and abdominal pain and had no previous medical history. The patient began experiencing abdominal distension 3 months prior, with intermittent abdominal pain and nausea developing after the first month. As symptoms persisted, the patient consulted the nearby clinic and underwent upper and lower gastrointestinal endoscopy and abdominal CT scan. Findings suggested ileal intussusception, and the patient was referred to our department for detailed examination.
The abdomen was flat and soft, and did not show tenderness or rebound tenderness. There were no palpable abdominal masses or Dance signs.
Abdominal contrast CT scan showed edematous thickening of the distal ileum (Fig. 1a), and we observed intussusception developing from a tumor lesion, with fat in the same site (Fig. 1b). Mild dilation was observed in the upper gastrointestinal tract, and there were no obvious regions of poor contrast. Based on these findings, the patient was diagnosed with intussusception of the ileum. As there were no findings suggesting gastrointestinal obstruction or impeded blood flow in the intestinal tract, the patient was scheduled for naval single-incision laparoscopically-assisted partial ileectomy.
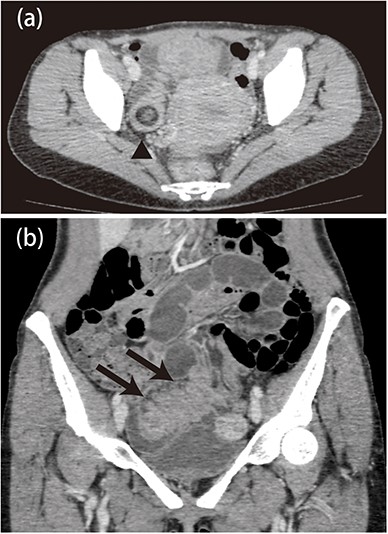
a: Abdominal computed tomography image showing an edematous and thickened ileum with advanced intussusception of the fat tissue. b: There was mild dilatation of the proximal side of the ileum, but no ischemic changes in the intestines.
Laparoscopy was performed by making a vertical incision measuring 3 cm in the navel. A wound retractor was inserted, and we laparoscopically observed the peritoneum via the suspension method until we located the lesion. The intestinal tract was brought out through the incision, and a mass was palpable in the lumen about 50 cm from the end of the ileum. An inversion in the opposite side of the upper gastrointestinal mesentery was thought to be the base of the mass, and we removed approximately 8 cm of the ileum, including this section (Fig. 2).

Intraoperative findings. Approximately 8 cm of the ileum was resected, including a mass lesion, which was palpated in the 50 cm ileum from a terminal ileum.
Examination of the mass showed protruding, raised lesions from the opposite side of the ileal intestinal mesentery to the intestinal lumen, which was considered to be an MD inversion. Furthermore, despite observing erosion at the top and sides of the diverticulum, no tumor or ectopic tissues were observed macroscopically (Fig. 3).

Meckel’s diverticulum was inverted and appeared as a polypoid lesion protruding toward the gut lumen. In addition, erosion was observed in the front and side of the diverticulum.
Histopathological examination revealed a full-thickness true diverticulum (Fig. 4a), and an aggregation of tall columnar epithelium, mucosal glands and islets of Langerhans were observed at the tip (Fig. 4b). Due to these findings, we concluded that the patient had ectopic pancreas with Heinrich Classification I [2].
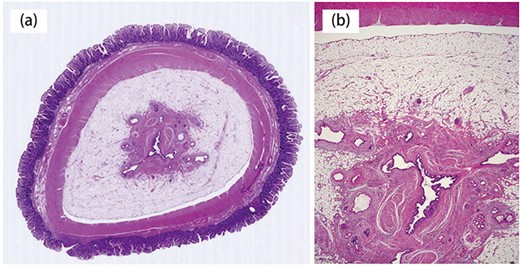
Histopathological findings. a:Diverticulum was a true diverticulum (hematoxylin and eosin stain). b: Specimen showing a high columnar, mucous epithelium; a mucous gland and insular colonization in the tip of the diverticulum.
The patient recovered well, resumed eating 3 days after surgery and was discharged 9 days after surgery.
DISCUSSION
We believe the case of intussusception presented here was caused by inversion of MD, with Heinrich I ectopic pancreas protruding into the intestinal tract. MD is believed to form from the remnant of the vitelline duct and is observed in 1–2% of autopsies. Reported complications of MD include intestinal obstruction, diverticulitis, intussusception and hemorrhagic ulcers. Of these, intussusception occurs in 13.2% of cases [3]. Adult-onset intussusception accounts for 5% of all intussusception cases, with almost half of those caused by malignant tumors [4].
Past reports have indicated that intussusception cases are more common in men (male-to-female ratio: 2.9:1), and the average age at onset is 40 years [5]. On average, the site of onset is 71.6 cm proximal to the ileocecal valve [5]. Furthermore, intussusception due to MD has rarely been diagnosed preoperatively, and many cases are found surgically due to other diagnoses including, but not limited to, intussusception alone, intussusception starting from small bowel tumors and appendicitis [6]. Histopathological findings of aberrant ectopic tissue in resected samples commonly show gastric mucosa, pancreatic tissue or both. However, some findings have also shown neither [7]. Aberrant pancreatic tissue (like that in the present case) is rarely seen, and many cases are only found after partial ileectomy based on the diagnosis of intussusception presenting with abdominal pain [6].
Generally, this condition is difficult to definitively diagnose prior to surgery. Motomura et al. proposed a CT scan of three layers at the intussusception development site as a possible preoperative diagnostic method [8]. A positive diagnosis of ectopic pancreatic tissue by CT scan includes (1) an iso-absorption area (wall of MD) that forms a ring surrounding (2) a low-absorption fat concentration region prevalent in MD, as well as (3) an iso-absorption region in the middle of the fat region.
Furthermore, Shimizu et al. proposed preoperative small bowel endoscopy for preoperative diagnosis and lesion-marking, which simplifies lesion identification during surgery [9]. In our case, diagnosing intussusception by imaging was straightforward. Intussusception developed from a tumor lesion with clear margins exhibiting fat concentration in CT scans. The patient was subsequently diagnosed with small intestine lipoma. However, considering that our patient was available for elective surgery, we believe it may have been feasible to reach a definitive diagnosis through detailed preoperative small bowel endoscopy.
Surgical resection is the standard treatment method in adult intussusception cases developing secondary to other conditions [10]. According to past reports, 3–6% of MD cases arise from a tumor, and there are also cases that have developed cancer from ectopic pancreatic tissue [7]. For this reason, intestinal resection by either laparotomic or laparoscopic surgery is the ideal approach. However, cases utilizing laparoscopic techniques, like ours, are typically free of postoperative complications, which is why we believe that laparoscopically-assisted surgery is safer and more effective than laparotomy. Furthermore, combining preoperative CT for identifying the site of interest with naval single-incision laparoscopy not only allows for straightforward confirmation of the lesion, but also improves consistency.
In conclusion, we report an adult case of MD inversion with ectopic pancreas, which developed into intussusception at the same site. The condition was treated by naval single-incision laparoscopically-assisted partial ileectomy.
Conflict of interest
All authors declare that there is no conflict of interest.



