-
PDF
- Split View
-
Views
-
Cite
Cite
Ana Sánchez-Gollarte, Jose María Mugüerza-Huguet, Manuel Mariano Díez-Alonso, Enrique Ovejero-Merino, Fernando Mendoza-Moreno, Pilar Hernández-Juara, María Esther López-Ramos, Fernando Noguerales-Fraguas, Septic thrombosis of internal jugular vein: a rare cause of uncontrollable hiccups, Journal of Surgical Case Reports, Volume 2019, Issue 9, September 2019, rjz266, https://doi.org/10.1093/jscr/rjz266
Close - Share Icon Share
Abstract
Septic thrombosis of the internal jugular vein is a possible complication related to central venous catheters. The enlargement of the diameter of the jugular vein can stimulate phrenic nerve causing hiccups and, septic thrombus can metastasize to different organs threating patient’s life. Diagnosis of septic thrombosis of internal jugular vein should be confirmed with a cervicothoracic CT-scan. Its management consists of catheter’s removal, antibiotic treatment and anticoagulation in high-risk patients. Surgical intervention might be considered if conservative treatment fails.
Introduction
Central venous catheters (CVCs) are widely used for nutritional aims after abdominal surgery. Pneumothorax, infection and thrombosis are common associated complications, but hiccup is rare. We report a case of uncontrollable hiccups presenting as the main symptom related to a septic thrombosis of the internal jugular vein after central venous access catheterization.
Case report
A 70-year-old male, with history of hypertension, diabetes and auricular fibrillation in treatment with oral anticoagulation, was diagnosed of adenocarcinoma of the sigmoid colon stage T4aN1M0. Laparoscopic exploration showed a perforated neoplasm of the sigma infiltrating terminal ileum and right colon. The procedure was reconverted to open surgery, and a total oncologic colectomy with ileo-rectal stapled anastomosis was performed.
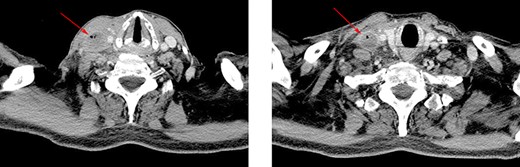
Axial CT view. Image shows a large diameter of right internal jugular vein and air bubbles inside the vessel.
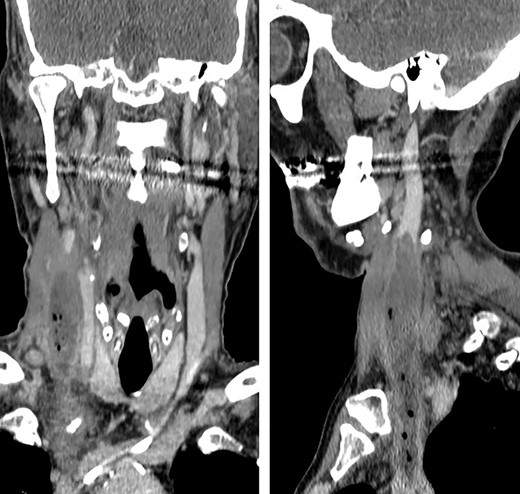
Coronal and sagittal images showing the jugular thrombosis along the neck.
Forty-eight hours later, the patient presented self-limited abdominal bleeding probably related to high dose of low molecular weight heparin (LMWH), which was treated conservatively. At the same time, hiccups appeared. It initially responded positively to haloperidol and chlorpromazine, but it progressed in frequency and intensity, becoming uncontrollable. A CT scan confirmed the absence of intraabdominal complication, and the patient was admitted to the intensive unit care to intensify hiccup treatment. During the next days, he started with fever peaks. Bacteraemia related to CVC was diagnosed, as well as inflammatory signs on the right jugular venous access. Due to the previous findings, a cervicothoracic CT was performed showing a thrombus and air bubbles into the right jugular vein. This conditioned a dilatation of an area of the vein intimately related to the phrenic nerve.
Considering persistent hiccups secondary to septic thrombosis of the jugular vein as the final diagnosis, treatment with LMWH and antibiotics was initiated. Catheter removal raised doubts because of its proximity to right auricula, so it was not initially removed. One week later, the patient was discharged from the intensive care unit to surgery ward. During next days, he presented isolated fever peaks which disappeared after catheter removal. A 3 weeks’ intravenous antibiotic cycle was performed, and the patient was discharged from the hospital.
Discussion
Hiccup is a common entity, usually self-limited and without any clinical repercussions. However, if it continues over time, it can be a sign of an underlying disease.
Hiccups’ reflex mechanism is based on an afferent pathway (phrenic, vagus nerve and other visceral sympathetic fibers), a central processor located at the periaqueductal gray area and the subthalamic nucleus and an efferent limb travelling from the brain within the phrenic nerve to the diaphragm and accessory nerves to intercostal muscles [1, 2, 4]. The stimulation of these structures leads to a quick contraction of the diaphragm and the intercostal muscles, followed by laryngeal closure [1]. Therefore, chemical and physical agents, or inflammatory and neoplastic status can stimulate any of these structures and cause hiccups [1, 2, 4].
Different agents have been associated to hiccups etiology, which stimulate central or peripheral structures of the hiccups’ reflex arc [1, 2, 4]. Some of these agents, such as trauma, tumors, infections or metabolic diseases, produce persistent hiccups (lasting more of 48 hours) or even untreatable (2 or more months lasting) [1, 4]. In this patient, hiccup etiology was difficult to identify and resulted in a diagnostic challenge, because fever and cervical inflammatory signs appeared days after hiccups. When signs and symptoms came together, a cervical TC was performed, concluding that manipulation of CVC led to a septic thrombosis of internal jugular vein, its dilatation and, finally, the direct compressive stimulation of phrenic and vagus nerves (Figs. 1 and 2). Topaz et al described a case of uncontrollable hiccups after the insertion of a catheter into jugular internal vein because of the compression of phrenic nerve due to a hematoma [2, 3].
Hiccup etiology was not the only diagnostic and therapeutic challenge, but also the septic thrombosis of internal jugular vein and the prevention of complications related to it. Septic thrombophlebitis of internal jugular vein, also called Lemierre syndrome, is an uncommon disease which usually occurs secondary to oropharyngeal infections, although in this case it was associated with the manipulation of a CVC [5]. Its diagnosis should be suspected in the presence of fever and painful cervical oedema after an acute pharyngoamygdalitis. The most serious and potentially life-threatening complications are distant septic metastasis, usually affecting lungs, but also other tissues such as bone, joints, skin, soft tissues and the central nervous system [5, 6].
Many drugs have been tried to treat persistent hiccups. Chlorpromazine is the most commonly used to this aim [1, 4]. However, other antidopaminergic drugs such as droperidol and metoclopramide can also be used to achieve an antiemetic postoperative effect. Other therapeutic options include baclofen and gabapentin, although they have a more gradual effect [1].
Treatment of etiological cause was added to symptomatic treatment of hiccups. However, the approach of the internal jugular vein septic thrombophlebitis remains controversial. It is accepted that infection must be treated using antibiotics against anaerobic bacteria, Streptococcus and Staphylococcus. Beta-lactamic antibiotics associated with beta-lactamase inhibitors are recommended as the first treatment option [5, 6]. The use of anticoagulant therapy is controversial because it could boost septic spread [5, 6]. In that sense, anticoagulation is used in case of high risk factors: trombophilia, lack of improvement even with correct antibiotic therapy, septic retrograde extension through internal jugular vein or thrombosis of the sigmoid sinus [5, 6]. The anticoagulant therapy and the length of treatment also remain controversial, although LMWH for 1–3 months is often used. In this case, the patient was already under anticoagulation therapy because of atrial fibrillation. Surgical treatment is recommended in case of clinical deterioration, abscess formation, septic embolism or large septic thrombosis [6].
In conclusion, persistent hiccups can be the first or the most evident manifestation of a nonsuspected disease, in this case a septic thrombophlebitis of the internal jugular vein related to a CVC. If hiccups appear during the post-operative period, peri-operative complications may be investigated, not only complications associated with surgery but also those which are related to anesthetic drugs or procedures. Diagnostic research may be directed to find the right etiology, so that the success of the treatment depends as much from symptomatic control as from the correct approach to the underlying disease.
CONFLICT OF INTEREST STATEMENT
None declared.



