-
PDF
- Split View
-
Views
-
Cite
Cite
Daiki Morita, Hitoshi Nemoto, Tomoichiro Togo, Naohiro Kimura, Yoshinori Ito, Skin ligation and argon beam coagulation for giant pachydermatocele resection, Journal of Surgical Case Reports, Volume 2019, Issue 9, September 2019, rjz264, https://doi.org/10.1093/jscr/rjz264
Close - Share Icon Share
Abstract
Resection of giant neurofibroma in neurofibromatosis type 1 has a high risk of perioperative bleeding because the tumors are enriched in blood vessels, which are weakened due to the loss and thinning of vascular smooth muscle. Therefore, we combined skin ligation around the tumor and use of an argon beam coagulator (ABC) for hemostasis during resecting the giant neurofibroma. The ABC is a non-contact-type hemostasis device employing argon gas as a medium. We examined the usefulness of our method by retrospectively comparing the outcomes of the ABC-use group with those of the non-use group (7 patients, 9 tumors). Although there was no difference in resected tumor weight between the two groups, the operation time was slightly shorter and the volume of blood loss was smaller in ABC-use group than in the non-use group. Our method for hemostasis is easy and safe and is considered to be a useful method.
INTRODUCTION
Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder, whose main symptoms are multiple scattered pigment spots and neurofibroma [1]. Resection of giant neurofibroma has a high risk of hemorrhage because of rich blood vessels in tumors and weakening of the blood vessels due to the loss and thinning of vascular smooth muscle [2, 3]. Therefore, we introduced a method to control intraoperative bleeding by combining skin ligation around the tumor and use of an argon beam coagulator (ABC) for resection of giant neurofibroma. The ABC is an energy device that induces hemostasis by causing a high-frequency current to reach the tissue in a non-contact manner using argon gas as a medium, and it is used for hemostasis in many medical departments [4–6]. We evaluated the usefulness of this method by comparing the outcomes of the ABC-use group with those of the non-use group.
CASE REPORT
Seven patients were diagnosed with NF1 at the Department of Plastic Surgery in the 17 years from January 2001 until December 2017 and underwent surgical resection for giant pachydermatocele (over 8 cm). We divided the patients into the ABC-use group and non-use group and retrospectively compared them for patient background, operation time and blood loss volume based on medical records. This study was approved by the Ethics Committee of our institution and Online Opt Out. In surgery, the skin around the tumor to be resected was first ligated, and the tumor was resected using ABC for hemostasis as needed.
Nine surgeries were performed for seven patients (Table 1). Patients were divided into the ABC-use group and non-use group, and the operative results were compared (Table 2).
| Case . | Age . | Sex . | Location . | Size (cm) . | Ligation . | ABC . | Autologous blood . | Transfusion . |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | Female | Buttock | - | None | Not used | Prepared | None |
| 2 | 70 | Male | Back | - | None | Not used | None | Done |
| 72 | Back | - | None | Not used | None | Done | ||
| 3 | 66 | Female | Face | 8 | None | Not used | None | None |
| 4 | 41 | Male | Face | 11 | None | Not used | None | None |
| 5 | 30 | Female | Occipital | 15 | None | Use | None | None |
| 6 | 20 | Female | Buttock | 17 | Done | Use | Prepared | None |
| 25 | Buttock | - | Done | Not used | Prepared | None | ||
| 7 | 53 | Female | Buttock | 17 | Done | Use | None | None |
| Average | 46.8 | 13.6 |
| Case . | Age . | Sex . | Location . | Size (cm) . | Ligation . | ABC . | Autologous blood . | Transfusion . |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | Female | Buttock | - | None | Not used | Prepared | None |
| 2 | 70 | Male | Back | - | None | Not used | None | Done |
| 72 | Back | - | None | Not used | None | Done | ||
| 3 | 66 | Female | Face | 8 | None | Not used | None | None |
| 4 | 41 | Male | Face | 11 | None | Not used | None | None |
| 5 | 30 | Female | Occipital | 15 | None | Use | None | None |
| 6 | 20 | Female | Buttock | 17 | Done | Use | Prepared | None |
| 25 | Buttock | - | Done | Not used | Prepared | None | ||
| 7 | 53 | Female | Buttock | 17 | Done | Use | None | None |
| Average | 46.8 | 13.6 |
| Case . | Age . | Sex . | Location . | Size (cm) . | Ligation . | ABC . | Autologous blood . | Transfusion . |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | Female | Buttock | - | None | Not used | Prepared | None |
| 2 | 70 | Male | Back | - | None | Not used | None | Done |
| 72 | Back | - | None | Not used | None | Done | ||
| 3 | 66 | Female | Face | 8 | None | Not used | None | None |
| 4 | 41 | Male | Face | 11 | None | Not used | None | None |
| 5 | 30 | Female | Occipital | 15 | None | Use | None | None |
| 6 | 20 | Female | Buttock | 17 | Done | Use | Prepared | None |
| 25 | Buttock | - | Done | Not used | Prepared | None | ||
| 7 | 53 | Female | Buttock | 17 | Done | Use | None | None |
| Average | 46.8 | 13.6 |
| Case . | Age . | Sex . | Location . | Size (cm) . | Ligation . | ABC . | Autologous blood . | Transfusion . |
|---|---|---|---|---|---|---|---|---|
| 1 | 44 | Female | Buttock | - | None | Not used | Prepared | None |
| 2 | 70 | Male | Back | - | None | Not used | None | Done |
| 72 | Back | - | None | Not used | None | Done | ||
| 3 | 66 | Female | Face | 8 | None | Not used | None | None |
| 4 | 41 | Male | Face | 11 | None | Not used | None | None |
| 5 | 30 | Female | Occipital | 15 | None | Use | None | None |
| 6 | 20 | Female | Buttock | 17 | Done | Use | Prepared | None |
| 25 | Buttock | - | Done | Not used | Prepared | None | ||
| 7 | 53 | Female | Buttock | 17 | Done | Use | None | None |
| Average | 46.8 | 13.6 |
| . | ABC-use group . | Non-use group . | P-value . |
|---|---|---|---|
| mean ± SD | mean ± SD | ||
| Resected tumor weight (g) | 580.5 ± 248.2 | 535.6 ± 552.7 | 0.54 |
| Operation time (min) | 99 ± 53 | 176 ± 67 | 0.0857 |
| Blood loss (ml) | 91.7 ± 33.3 | 1152.3 ± 1343 | 0.055 |
| Hospitalization (day) | 12.7 ± 6.7 | 17.8 ± 5.8 | 0.134 |
| . | ABC-use group . | Non-use group . | P-value . |
|---|---|---|---|
| mean ± SD | mean ± SD | ||
| Resected tumor weight (g) | 580.5 ± 248.2 | 535.6 ± 552.7 | 0.54 |
| Operation time (min) | 99 ± 53 | 176 ± 67 | 0.0857 |
| Blood loss (ml) | 91.7 ± 33.3 | 1152.3 ± 1343 | 0.055 |
| Hospitalization (day) | 12.7 ± 6.7 | 17.8 ± 5.8 | 0.134 |
SD: standard deviation.
| . | ABC-use group . | Non-use group . | P-value . |
|---|---|---|---|
| mean ± SD | mean ± SD | ||
| Resected tumor weight (g) | 580.5 ± 248.2 | 535.6 ± 552.7 | 0.54 |
| Operation time (min) | 99 ± 53 | 176 ± 67 | 0.0857 |
| Blood loss (ml) | 91.7 ± 33.3 | 1152.3 ± 1343 | 0.055 |
| Hospitalization (day) | 12.7 ± 6.7 | 17.8 ± 5.8 | 0.134 |
| . | ABC-use group . | Non-use group . | P-value . |
|---|---|---|---|
| mean ± SD | mean ± SD | ||
| Resected tumor weight (g) | 580.5 ± 248.2 | 535.6 ± 552.7 | 0.54 |
| Operation time (min) | 99 ± 53 | 176 ± 67 | 0.0857 |
| Blood loss (ml) | 91.7 ± 33.3 | 1152.3 ± 1343 | 0.055 |
| Hospitalization (day) | 12.7 ± 6.7 | 17.8 ± 5.8 | 0.134 |
SD: standard deviation.
Case 7: a 53-year-old female
First, the skin around the tumor to be resected was ligated. Silk threads were used to penetrate the skin in an X shape and were ligated. Thereafter, tumor resection was performed, and hemorrhage was managed using the ABC as needed (Fig. 1). A negative pressure drain was placed in the resected space, and compression fixation was made.
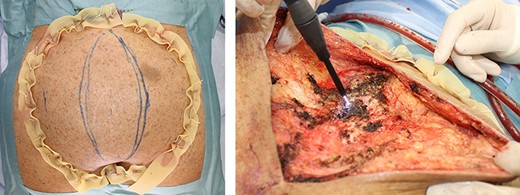
Operative view for Patient 7. Left: the skin around the tumor to be resected was ligated by inserting silk thread in an X shape. This temporarily decreases the blood flow to the tumor from the skin. Right: hemostatic procedure using the ABC.

Operative view for Patient 6. The skin near the base of the tumor to be resected was ligated by inserting silk thread.
Case 6: a 20-year-old female
First, the skin near the base of the tumor to be excised was pierced and ligated with silk thread (Fig. 2). The tumor was then resected while performing hemostasis using the ABC as needed.
DISCUSSION
Pachydermatocele in NF1 gradually increases in size, and when the tumor hangs pendulously, aesthetic and functional disorders occur. As a result, the quality of life of the patient may decrease. As large pachydermatocele has a risk of intratumoral hemorrhage caused by vascular fragility and secondary malignant peripheral nerve sheath tumors, early surgical resection is desirable before the tumor increases in size. However, these tumors have fragile supportive tissue and rich blood vessels, which are delicate. There is a risk of marked hemorrhage at the time of resection. Therefore, for hemostasis in NF1 patients, contact-type instruments, such as conventional monopolar and bipolar systems, increase the possibility of a blood clot adhering to the tip and peeling off when detached, causing hemorrhage.
Evaluation of tumors by image examinations, such as magnetic resonance imaging and angiography, and embolization before surgery are considered effective [7]. Preoperative embolectomy has problems in that the number of treatments increases and the dermal necrosis may occur. Thus, the use of ultrasonic coagulation and incising devices or special electric coagulation and incising devices for tumor resection has been reported [8, 9]. However, these devices extend the operation time and sufficient skills are needed for their use.
Therefore, we introduced the method of ligating the skin around the tumor and using the ABC for hemostasis as a countermeasure against hemorrhage when resecting a pachydermatocele. Ligation of the skin around the tumor is expected to temporarily reduce the blood flow to the tumor from the skin. Maeda et al. [10] reported a similar method of ligation around the tumor using a Tsukisui device during neurofibroma resection. Ligation using a Tsukisui device is simple and can be used as a substitute for the skin ligation around the tumor following our method. Our method of conducting hemostasis with the ABC at the time of resection is considered to be a more effective countermeasure for bleeding.
ABC is a non-contact-type electric hemostatic device using argon gas as a medium. The ABC can (i) provide effective coagulation of the target site with reduced eschar because the outflow of argon gas blows off the blood and (ii) minimize tissue damage in a shallow coagulation area because coagulation is rapid. Since Ward et al. [4–6] first used ABC for head and neck operations, its use has been reported from several medical departments.
Due to these characteristics, the ABC is effective for extensive and fragile tissue, and micro-blood vessel coagulation. However, because the eschar layer is shallow, there is a risk of hemorrhage after hemostasis for pulsatile bleeding. In addition, because ABC cauterizes on the surface and not at a point like a laser, it may take more time to acquire tissue adhesion when ABC is used extensively. In Patient 7, the wound was partially pocketed, and adhesion required a longer time than usual.
In the ABC-use group, although not significant, the operative time was slightly shorter and the volume of blood loss was smaller. There was no difference in resected tumor weight. The volume of blood loss was reduced and the operation time was shortened because this method improved the hemostasis procedure. Prior to using this method, autologous blood was taken before tumor resection according to the risk of hemorrhage. However, because bleeding control was not difficult, autologous blood did not need to be prepared.
The combined use of skin ligation around the tumor and the ABC is simple and safe and is considered to be useful as a method of hemostasis for resection of giant neurofibromas in NF1.
We evaluated the utility of skin ligation around the tumor and the use of the ABC for hemostasis when resecting giant pachydermatocele in NF1 patients. Sufficient hemostasis was possible using this method.
Conflict of interest statement
None declared.
Funding
No source of funding.



