-
PDF
- Split View
-
Views
-
Cite
Cite
Akio Sakamoto, Takeshi Okamoto, Shuichi Matsuda, A posterior approach for curettage in giant cell tumor of bone in the proximal fibula, Journal of Surgical Case Reports, Volume 2019, Issue 9, September 2019, rjz252, https://doi.org/10.1093/jscr/rjz252
Close - Share Icon Share
Abstract
Giant cell tumor of bone (GCTB) is a locally aggressive tumor. En bloc resection to reduce the recurrence rate has a high risk of peroneal nerve paralysis and knee instability associated with collateral ligament resection. In the current report, the posterior approach to curettage is introduced in a 55-year-old male with GCTB in the proximal fibula. The approach makes a wide operative field for curettage of GCTB in the proximal fibula without dissecting the peroneal nerve. The approach would prevent postoperative peroneal nerve palsy and knee instability and possibly reduce recurrences.
INTRODUCTION
Giant cell tumor of bone (GCTB) is a locally aggressive, benign tumor, occurring in patients aged 20–45 years. The tumors occur in the metaphysis to the epiphysis [1]. The most common location is around the knee joint, and the proximal fibula is a rare location for GCTB. In cases with GCTB in the proximal fibula, a high recurrence rate after curettage and bone grafting has been reported. Therefore, en bloc excision of the tumor is the treatment of choice for GCTB in the proximal fibula [2–4].
Peroneal nerve palsy is a serious postoperative complication associated with resection of the tumors at the fibular head. The incidence rate of peroneal nerve palsy ranges from 7 to 57% and is higher after en bloc resection than curettage [2, 5, 6]. When an en bloc resection of the fibular head is accompanied by a lateral collateral ligament resection, reconstruction is necessary [5], though the need for reconstruction is controversial [7].
In order to reduce the concerns about nerve palsy and knee instability, curettage would be preferable to en bloc resection. In the current case, a safe posterior approach for the proximal fibula is introduced to allow for sufficient exposure of the operative field for curettage, possibly leading to a low recurrence rate.
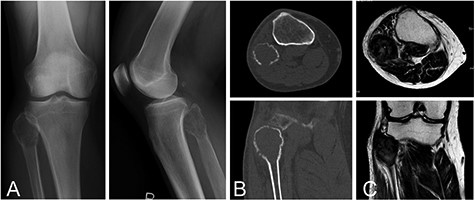
A 55-year-old male with GCTB in the proximal fibula. Plain radiographs (A) and computed tomography (B) show an osteolytic and expansive lesion. On magnetic resonance imaging, the lesion has a heterogeneous low-to-intermediate signal intensity on the T2-weighted image (C)
CASE PRESENTATION
The patient was a 55-year-old male. He had noticed a pain in the left proximal lower leg 3 months earlier, after jumping from a 50 cm height. The patient was referred to our institute on the diagnosis of bone tumor. The pain had disappeared 1 month after the injury. Physical examination revealed no swelling and slight tenderness at the fibular head. Laboratory studies showed no remarkable findings. A plain radiograph and computed tomography showed an expansive and osteolytic lesion, involving the proximal fibular head (Figs. 1A and B). Magnetic resonance imaging of the lesion showed homogenous intermediate signal intensity on a T1-weighted image and heterogeneous low-to-intermediate signal intensity on a T2-weighted image (Fig. 1C). Based on the results of a needle biopsy, the diagnosis of GCTB was confirmed.
Resection was performed with the patient in the lateral position, and the common peroneal nerve was identified under the fascia. The posterior surface of the proximal fibula was exposed by retracting the soleus muscle from the posterior cortex (Fig. 2A). The cortex over the lesion was fenestrated, and the lesion was curetted. After curettage of the lesion, the cavity was filled with ethanol for 5 minutes as adjuvant therapy, for the purpose of decreasing a possible recurrence. Then, β-tricalcium phosphate particles were implanted (Fig. 2B). A local recurrence was not observed at 12 months postoperatively, and bone incorporation was seen. The range of motion in the knee was not restricted on distal flexion, and there were no complications.
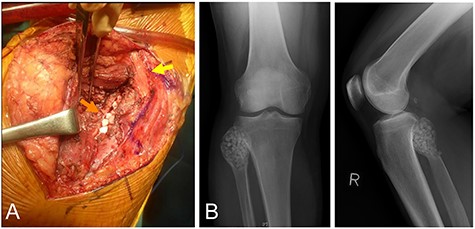
The same patient as in Fig. 1. Posterior approach to the proximal fibula. Note the common peroneal nerve was not dissected from the fibular head (yellow arrow), and β-tricalcium phosphate (β-TCP) particles were implanted from the posterior (orange arrow) (A), with retraction of the soleus muscle posteriorly. Postoperative plain radiographs after β-TCP particles were implanted in the cavity (B).
DISCUSSION
In the current case, we report a posterior approach for curettage performed by detaching the soleus muscle and exposing the posterior side of the proximal fibula. Peroneal nerve palsy is a serious postoperative complication associated with resection of these tumors at the fibular head. Despite protective measures, previous studies have revealed a high rate of iatrogenic peroneal nerve palsy, especially after en bloc resection [5, 6]. The common peroneal nerve runs on the lateral surface of the proximal fibula, and the nerve is elevated and stretched due to tumor extension of the fibular head [2]. Retraction of the nerve seemed to make it susceptible to palsy in en bloc resection of the proximal fibula. Moreover, the nerve could be adherent to the adjacent, tumor-affected bone; thus, dissection itself would be a risk factor for peroneal nerve palsy. The current posterior approach is characterized by no necessity for dissecting the nerve from the lateral surface of the fibula, which would decrease the possibility of nerve palsy from the surgery.
The problem with curettage for GCTB in the proximal fibula is a high recurrence rate [2–4]. A low recurrence rate after en bloc resection of GCTB located in the proximal fibula has been reported, and en bloc resection rather than curettage is recommended [2]. Adjuvant therapy could reduce the recurrence rate in GCTB. In the current case, ethanol was used as the adjuvant, and the previously reported recurrence rate with ethanol was 9.5% in overall GCTB [8]. Even with usage of adjuvant therapy after curettage, local recurrences occurred in two of four cases of GCTB [7]. The high recurrence rate of GCTB in the fibular head may be because of anatomic complexity and difficult extension of the operative field. The current posterior approach would easily make a wide operative field for curettage by dissection of the soleus muscle, possibly leading to a low recurrence rate. In this case, surgery was performed with the patient in the lateral position; however, surgery could be done with the patient in the prone position, so that it is easy to administer ethanol in the cavity for adjuvant therapy.
The lateral collateral ligament is an important structure in relation to bone tumors in the proximal fibula [9]. After en bloc resection of the proximal fibula with the ligament, postoperative knee instability is a concern [2, 10]. The need for reconstruction of the ligament is controversial [7]. However, the lateral collateral ligament and the biceps femoris tendon are attached to the fibular head, and both structures determine the laxity of the knee. Also, it has been reported that repair of not only the lateral collateral ligament but also the biceps femoris tendon is necessary after en bloc resection of the fibular head [2].
Because of the anatomic complications, the following are concerns after en bloc resection of GCTB located in the proximal fibula: peroneal nerve palsies, knee stability and local recurrence. This report describes the posterior approach for curettage in GCTB in the proximal fibula. This approach makes a wide operative field for curettage without the necessity of dissecting the nerve from the fibular head. The approach may possibly reduce recurrences and prevent two main adverse outcomes: postoperative peroneal nerve palsy and knee instability.
Conflict of interest statement
None declared.



