-
PDF
- Split View
-
Views
-
Cite
Cite
Yoko Amano, Yusuke Takanashi, Hiroshi Neyatani, Emergency left pneumonectomy for foreign body aspiration: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 9, September 2019, rjz258, https://doi.org/10.1093/jscr/rjz258
Close - Share Icon Share
Abstract
Bronchoscopic extraction is the most common treatment of foreign body aspiration. However, surgical interventions are required in cases wherein bronchoscopic extraction is difficult, with the most frequent surgical strategy being bronchotomy or lobectomy. Herein, we report a case of foreign body aspiration wherein left pneumonectomy was inevitable because of a molar incarcerated in the left main bronchus. The large diameter of the foreign body and delayed diagnosis that causes granulomatous hyperplasia are considered to be major factors of requiring high invasive surgery.
Introduction
Bronchoscopic extraction is the most preferred treatment of foreign body aspiration (FBA). However, surgical intervention is required in cases wherein bronchoscopic extraction of the foreign body is complicated. Although bronchotomy and lobectomy are the common surgical modalities in such cases, the cases that require pneumonectomy are rare. Herein, we present a rare case of FBA, in which a molar was incarcerated in the left main bronchus, making left pneumonectomy inevitable.
Case Report
A 72-year-old man, bedridden with aphasia because of a medical history of stroke, was referred to our hospital because of high fever and hypoxemia. Chest X-ray and chest computed tomography (CT) demonstrated a 12- × 17-mm foreign body, in the left main bronchus, which appeared to be a tooth from its shape and high-density equivalent to that of a bone (Fig. 1a, arrow). The bronchial wall in contact with the foreign body was hypertrophic, and the left lung showed broad atelectasis (Fig. 1b, arrows). Laboratory studies revealed elevated values of white blood cell (15 600/μL) and C-reactive protein (12.62 mg/dL).
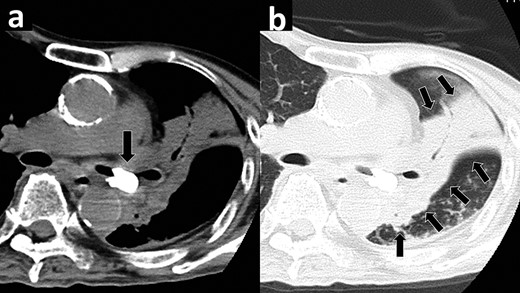
Chest computed tomography showing a bone density foreign body (arrow) in the left main bronchus (a). The left lung showing broad atelectasis (arrows) (b).
Under intubation with light sedation, bronchoscopy revealed the root of a tooth at the periphery of the left main bronchus with surrounding granulation. Endoscopic extraction of the tooth using Fogarty catheter and biopsy forceps was infeasible because of the granulation-caused dense adhesion. Therefore, we performed an emergency surgery to remove the foreign body and control infection. To preserve lung function, sleeve resection of the left upper or lower lobe was considered as one of surgical options. However, since the bronchial wall in contact with the foreign body was hypertrophic with strong inflammation, the patient was considered to be at high risk of anastomotic complication. Thus, we selected left pneumonectomy with bronchial transection at an inflammation-intact proximal left main bronchus.
The surgery was initiated with posterolateral thoracotomy. Intraoperatively, we could confirm the location of the tooth by manual sensing via the left main bronchial wall, and we could complete left pneumonectomy safely. The patient was extubated immediately after the surgery, and his oxygenation drastically improved. Surgical specimen observation revealed that the foreign body was a molar that rigidly adhered to the wall of the left main bronchus by hyperplastic granulation (Fig. 2, circle).
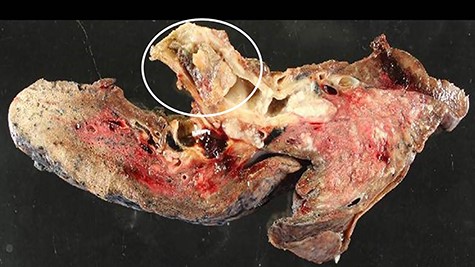
In the surgical specimen, a molar is undetachably adhered to the bronchial wall (circle).
The postoperative course was uneventful without hypoxemia or any symptoms of heart failure. A negative conversion of the inflammatory reaction was confirmed on postoperative day 7, and we terminated antibiotic treatment. The patient was discharged from the hospital on postoperative day 34.
Discussion
Probable cases of FBA, though asymptomatic, should be evaluated for the presence of granulomatous hyperplasia, indicative of more than 3 days since an active FBA.
Herein, we present a rare case of a bronchial foreign body, a molar, incarcerated in the left main bronchus, which required an emergent left pneumonectomy. Generally, the most frequently used surgical procedures for patients with FBA are bronchotomy and lobectomy [1]. However, pneumonectomy, a more invasive surgery that exceeds the frequent indications for surgical management, was required in our case. The patient was on the verge of developing a septic shock, and immediate treatment was required to control the patient’s pneumonia. As observed in the histopathological examination of the surgical specimen, the molar was strongly adhered to the bronchial wall. Therefore, a bronchoscopic extraction was impractical and surgical intervention was necessary. Although sleeve resection was considered to preserve lung function, the patient’s general condition seemed intolerable to a second operation after initially presenting with anastomotic complication. Thus, a left pneumonectomy was indisputably chosen for treatment.
The mean lumen diameter of the left main bronchus in men is 10–14 mm, whereas, that of the right main bronchus is wider (12–16 mm) [2]. Although foreign bodies often fall in right main bronchus, they commonly occlude the left main bronchus because of its narrower diameter in comparison to the right. Presently, the diameter of the aspirated molar was 13 mm, sufficient to occlude the left main bronchus. However, a diameter of <10 mm or it’s aspiration into the right main bronchus or been <10 mm in diameter could have enabled its passage into the peripheral bronchus, for which lobectomy can be performed.
When the presence of a >10-mm foreign body in the left main bronchus is diagnosed after 3 days of aspiration, performing a left pneumonectomy could have been effectively inevitable.
Although tracheobronchial FBA is a potentially fatal event that can occur in all age groups, it is more common among children and the elderly [3]. The diagnosis of FBA is easy when the medical history of aspiration is obvious or when the patients manifest definitive symptoms, such as choking. However, in cases of elderly patients with dementia or stroke, the symptoms may be weakly or non-specifically manifested, and the diagnosis can be delayed until they exhibit respiratory failure or infection because of the aggravation of FBA. During the diagnostic delay, FBA causes various complications, including pneumonia and hemoptysis.
Although there is no standard guideline for managing FBAs, bronchoscopic extraction is the first choice among all treatment modalities because of its low invasiveness in comparison with surgical treatments. However, the presence of dense adhesion because of granulomatous hyperplasia can complicate the bronchoscopic extraction of the foreign body. Moreover, delayed diagnosis and formation of granulomatous hyperplasia correlate positively. In cases of FBA that are diagnosed within 3 days since aspiration, the incidence of granulomatous hyperplasia is 22.3%. Contrarily, in FBA cases with delayed diagnosis (>3 days), the incidence of granulomatous hyperplasia increases to 83.1% [4]. Thus, bronchoscopic extraction of the FBA, >3 days after incarceration, can be difficult because of the granuloma formation.
In our case, the history of the tooth aspiration was not obvious because the patient had aphasia. Thus, the bronchial foreign body was not detected until deterioration of the non-specific symptoms, including fever and dyspnea. The molar was found to be undetachably adhered to the bronchial wall because of the granulomatous hyperplasia, indicative that more than 3 days had passed since the aspiration.
Conflict of interest statement
I declare on behalf of my co-authors and myself that we do not have any conflict of interest to declare.



