-
PDF
- Split View
-
Views
-
Cite
Cite
Mahmoud Labib, Asmaa Ismail, Hazem Elmansy, Walid Shahrour, Owen Prowse, Ahmed Kotb, Adrenalectomy for huge solid pheochromocytoma: a challenging surgery or piece of cake?, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz255, https://doi.org/10.1093/jscr/rjz255
Close - Share Icon Share
ABSTRACT
Pheochromocytoma (PCC) is an uncommon adrenal tumor that is occasionally diagnosed during the work up for patients with uncontrolled hypertension. Treatment of PCC is mainly surgical. This case represents the largest PCC reported to date, which was safely removed.
INTRODUCTION
Pheochromocytoma (PCC) is an uncommon adrenal tumor that is occasionally diagnosed during the work up for patients with uncontrolled hypertension. Treatment of PCC is mainly surgical with consideration of radiotherapy in unresectable cases [1]. Ambati et al. [2] reported a case for 19 cm PCC and described it as the largest PCC reported in Canada at that time.
CASE REPORT
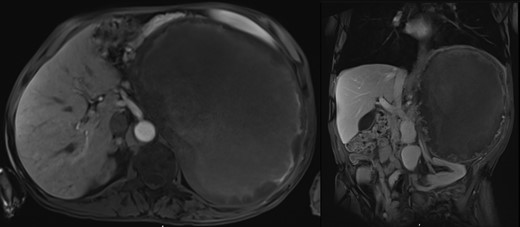
A seventy-four-year-old gentleman was referred with a left loin pain and a large abdominal mass. His symptoms included headaches, loss of appetite, chronic anemia and weight loss with a documented systolic blood pressure of over 200 mmHg. Abdominal examination showed an obvious large left abdominal mass. MRI scan showed a 25 cm left adrenal tumor (Fig. 1). Endocrinological lab work up was consistent with a PCC.
Anesthetic technique
Preoperative phase
The patient was seen approximately two weeks preoperatively. He was started on doxazosin 2 mg and the dose was increased daily by 1 mg targeting a systolic pressure of less than 130 mmHg with a postural drop. After reaching a maximum dose of doxazosin of 17 mg, his systolic pressure remained in the 150–160 mmHg range. The amlodipine was increased gradually to reach 20 mg.
Intraoperative phase
The patient was started on dexmedetomidine at 0.3 mcg/kg/h after receiving a bolus of 0.2 mcg/kg over 10 minutes. A radial arterial line was inserted, followed by a thoracic epidural sited at T4-5 and loaded with 10 cc of bupivacaine 0.1%. A 10 cc/kg bolus of Voluven was administered pre-induction. The patient was induced with midazolam 0.03 mg/kg, sufentanil 0.5 mcg/kg and Propofol 0.5 mg/kg. Endotracheal intubation was achieved successfully and anesthesia was maintained on sevoflurane and an epidural infusion of bupivacaine 0.1% at 6 cc/h. A right internal jugular triple lumen central line was inserted. The following infusions were in-line on the central line: nitroglycerine, nitroprusside, norepinephrine and vasopressin. The following medications were available for boluses: nitroglycerine, phentolamine, norepinephrine and vasopressin. There were no major hemodynamic changes during surgical manipulation. As expected, the patient encountered hypotension after ligating the venous supply of the tumor and required starting infusions of norepinephrine at 0.1 mcg/kg/min and vasopressin at.04 u/kg/h.
Surgical technique
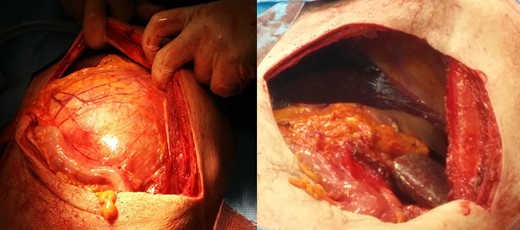
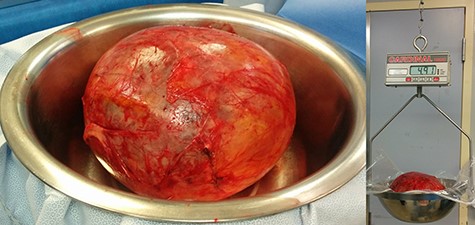
The patient was positioned in the supine position, with the left side elevated 30° and a chevron incision was done. The mass was immediately encountered, and the left colon was seen stretched over the mass. Our first step was complete kocherization of the colon and extended cautious medial dissection to the aorta. This was then extended downwards identifying and dissecting the renal pedicle. The long left suprarenal vein was identified and was double clipped. The dissection was then extended inferiorly dissecting the lower part of the adrenal gland from the kidney and then extended to the posterior surface of the adrenal gland. The dissection was then continued on the posterior and lateral surfaces of the adrenal gland using blunt dissection and Ligasure. The upper part of the adrenal gland had adherent spleen and distal pancreas that were dissected using monopolar cautery and sharp dissection. Once dissected, the stomach was found very adherent to the adrenal gland with abnormal vascular communication between them. These vascular attachments were meticulously dissected using monopolar cautery and sharp dissection. Left adrenalectomy could now be safely completed. Figure 2 shows our surgical approach before and after adrenalectomy. Blood loss was minimal, and the mass came out as a well encapsulated mass, weighted 4.91 kg (Fig. 3) and pathology found most of the mass formed of necrotic tissue.
DISCUSSION
PCC tumors present real anesthetic and surgical challenges. Preoperative treatment and optimization of hypertension are crucial as surgical manipulation of the tumor can precipitate severe hypertensive crisis causing catastrophic events including strokes and myocardial ischemia. Alpha blockade remains the mainstay for optimizing these patients with beta-blockade reserved only to control heart rate after alpha blockade has been established [3].
Giant PCC is very uncommon, and cases in the literature represent case reports and personal experience. Ambati et al. [2] reported their mass of 19 cm, but did not specify their surgical approach. Afaneh et al. [4] reported an 18 cm PCC that weighted less than 2 kg and was removed through a midline incision with left lateral extension. Gupta et al. [5] reported a case of 25 cm, 2750 g PCC, with the kidney removed along with the adrenal gland, but the surgical approach was not mentioned. Pan et al. [6] reported a case of 18 cm PCC. Maharaj et al. reported a case of a 23 cm PCC that was managed through a chevron incision and required en bloc nephrectomy, splenectomy and distal pancreatectomy. Ma et al. [6] reported a case of a 13 cm PCC and no mention of the surgical approach [7]. It was interesting that all these cases to date the giant PCC was mainly cystic. Ologun et al. [8] reported a case of 20 cm solid PCC, but did not mention their surgical approach.
Our case is unique in being the largest PCC reported in the literature to date and for being solid giant PCC with no cystic component. This patient was denied surgery in other centers before being referred to us. We think some skilled surgeons were concerned because of the mass size and assumed surgical difficulties. Based on our experience, huge adrenal masses including PCC can be safer to remove than smaller tumors; the reason is the lack of large arterial supply to the adrenal gland, which transforms most of the solid components of the gland into necrotic tissue and creates well encapsulated mass. Although CT scans usually give a gloomy picture and raise concerns towards adhesions to surrounding organs, the masses tend to be well encapsulated, and cautious dissection can allow for an adrenalectomy, while preserving the surrounding organs.
CONCLUSION
Open adrenalectomy for huge solid PCC tumors is safe and feasible in experienced hands. Meticulous preoperative optimization of patients and team work can allow safe surgery while preserving surrounding organs.
ACKNOWLEDGEMENT
We would like to acknowledge the great role of our operating nursing staff that was highly trained and efficient to allow safe successful surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
No source of funding.



