-
PDF
- Split View
-
Views
-
Cite
Cite
Geon Young Byun, Bum Hwan Koo, Seung Geun Lee, Myoung Jin Kim, Sung Ryul Lee, Laparoscopic removal of rare variant of leiomyoma in the female inguinal canal: a report of two cases, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz242, https://doi.org/10.1093/jscr/rjz242
Close - Share Icon Share
Abstract
Angioleiomyoma and lipoleiomyoma are rarely found tumors in the inguinal canal. We present two cases of laparoscopic removal of angioleiomyoma and lipoleiomyoma in the female inguinal canal. In Case 1, a 35-year-old woman was admitted to our hospital with left inguinal swelling and intermittent pain. A hypoechoic well-marginated mass was observed on ultrasonography. Laparoscopic complete tumor excision and posterior wall repair were performed, and a diagnosis of angioleiomyoma was confirmed on histopathological evaluation. In Case 2, a 55-year-old woman was admitted with a painful right inguinal swelling. A hypoechoic well-marginated ovoid mass was observed on ultrasonography. Laparoscopic complete tumor excision and posterior wall repair were performed, and a diagnosis of lipoleiomyoma was confirmed on histopathological evaluation. Laparoscopic tumor excision and posterior wall repair are effective treatments of leiomyomas in the inguinal canal.
INTRODUCTION
Angioleiomyoma is a leiomyoma occurring in a blood vessel and originating from the tunica media of the vessel wall [1]. It commonly occurs at the age of 40–60 years and is most often located in the superficial soft tissue of the lower extremities [2]. Lipoleiomyoma is a benign soft tissue tumor that was first described in 1991 [3]. It is a subtype of leiomyoma consisting of smooth muscle cells along with varying degrees of mature adipose tissue. Lipoleiomyoma usually occurs in the abdominal cavity and retroperitoneum. Most cases of inguinal bulging in female patients are caused by hernias or hydroceles. However, in the rare occurrence of an angioleiomyoma or lipoleiomyoma in the inguinal canal, the affected patient develops symptoms similar to those of hernias and hydroceles. We herein present two cases of laparoscopic removal of angioleiomyoma and lipoleiomyoma in the female inguinal canal.
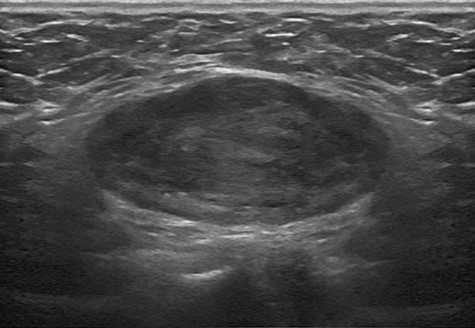
Ultrasonographic findings of the tumor in Case 1. A 9 × 3 cm hypoechoic, well-marginated mass was present in the left inguinal area.
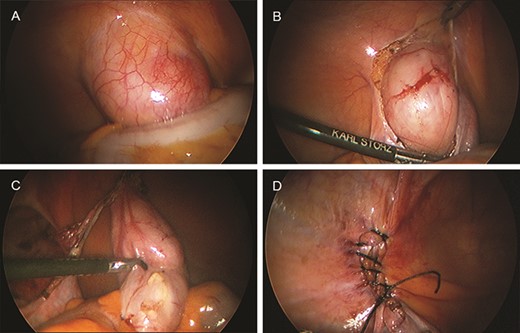
(A) Laparoscopic view of the internal ring. A round mass is evident. (B) Dissection of the peritoneum. (C) Complete excision of the tumor. (D) Closure of the internal ring.
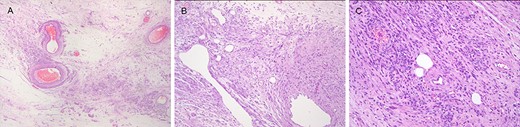
Pathologic findings of angioleiomyoma in the canal of Nuck. (A) Edematous background. (B) Spotty vascular congestion and venous proliferation of various sizes. (C) Differentiation in smooth muscle cell gathered with compact (hematoxylin and eosin staining).
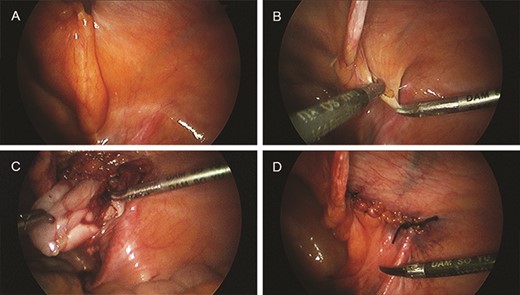
(A) Laparoscopic view of the internal ring. (B) Dissection of the peritoneum. (C) Complete excision of the tumor. (D) Closure of the internal ring.
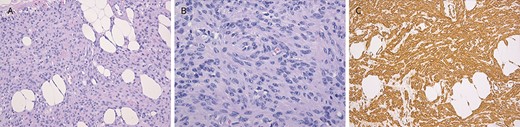
Pathologic findings of lipoleiomyoma in the canal of Nuck. (A) Diffuse solid monotonous cell proliferation intermixed with mature adipose tissue and myxoid edematous stroma is noted on hematoxylin and eosin staining. (B) Proliferative area of cellular spindle cells with elongated and vesicular nuclei and a lack of adipose tissue on hematoxylin and eosin staining. (C) Diffuse and strong positive reaction to proliferating tumor cells on smooth muscle actin staining.
CASE REPORT
Case 1
A 35-year-old woman was admitted due to left inguinal swelling with an intermittent pain that had begun 3 months previously. The patient had no significant medical, drug, smoking, trauma, abdominal surgery or family history. Physical examination revealed an approximately 9-cm soft, movable mass with mild tenderness. Ultrasonography revealed a hypoechoic well-marginated 9 × 3 cm ovoid mass in the left inguinal area (Fig. 1). The operation was performed under general anesthesia with the patient placed in a supine position. A 5-mm incision was made through the umbilicus down to the midline fascia for 5-mm 30° camera port. Two 3-mm incisions were made on both lateral sides of the abdomen for the instrument insertion. Laparoscopy showed that the internal ring was occluded, and the mass was displaced into the peritoneal cavity when the inguinal area was pressed from the outside. The tumor was easily separated from the surrounding tissues, and complete intracorporeal excision of the tumor and posterior wall repair were performed (Fig. 2). The histopathological evaluation confirmed a solid, well-marginated mass described as a stromal cell proliferative lesion with multifocal vascular ectasia and tangles of smooth muscle bundles (Fig. 3). The pathological diagnosis was angioleiomyoma. The patient was discharged the next day. Postoperative pain improved daily, and there was no postoperative wound infection, bleeding, or fluid collection observed. The patient was followed up for 1 week, 1 month, 6 months and 1 year after the discharge. The surgical site was assessed by ultrasonography. There was no evidence of recurrence 12 months after the surgery.
Case 2
A 53-year-old woman was admitted with a mildly painful right inguinal swelling that had begun 1 month previously. The patient had no significant medical, drug, smoking, trauma, abdominal surgery or family history. Physical examination revealed an approximately 5-cm soft, movable mass without tenderness. Ultrasonography revealed a hypoechoic well-marginated 6 × 3 cm ovoid mass in the right inguinal area. Laparoscopy showed that the internal ring was occluded. The tumor was easily separated from the surrounding tissues, and complete excision of the tumor and posterior wall repair were performed (Fig. 4). Histopathological evaluation confirmed a lipoleiomyoma with extensive myxoid degeneration. On immunohistochemical staining, the origin of the spindle cell component was a smooth muscle (Fig. 5).
The patient was discharged the next day. Postoperative pain improved daily, and there was no postoperative wound infection, bleeding or fluid collection observed. The patient was followed up for 1 week, 1 month, 6 months and 1 year after discharge. The surgical site was assessed by ultrasonography. There was no evidence of recurrence 12 months after the surgery.
DISCUSSION
Angioleiomyoma is a relatively rare type of leiomyoma originating from arterial and venous smooth muscle tissue. This soft tissue tumor often occurs in middle-aged women as a subcutaneous nodule in the lower extremities [4]. Hachisuga et al. [2] evaluated 562 patients with angioleiomyomas and reported that 67% were located in the lower extremities, 22% were located in the upper extremities, 8.5% were located in the head and neck and 2.5% were located in the trunk. Angioleiomyomas account for 4.4% of all benign soft tissue tumors [5]. The usual clinical presentation is a painful round, soft solitary nodule. Hachisuga et al. [2] reported that pain or tenderness was observed in 327 of 562 patients (58%). Our patients complained of pain when bending at the waist or standing for a long time. Normally, this condition can be examined by ultrasound or computed tomography; however, it may be difficult to diagnose because the symptoms are quite similar to those of inguinal hernia. The exact cause of angioleiomyomas is not known, but trauma and hormones have been discussed as potential etiologies [6].
Angioleiomyomas and lipoleiomyomas in the inguinal canal are rarely reported, and the swelling and presenting symptoms of our patients were initially attributed to an inguinal hernia. Distinguishing a lipoma in the canal of Nuck from an inguinal hernia is not easy using ultrasonography because they both show a homogenous structure with a well-defined margin [7]. Avritscher et al. [8] suggested that the tumor may arise from misplaced embryonic remains of lipoblasts or due to the perivascular extension of peritoneal or retroperitoneal fat. Lipoleiomyomas have also been reported in the cervix, broad ligament, retroperitoneum and ovary [9]. No specific imaging technique is available to diagnose angioleiomyoma. Magnetic resonance imaging is relatively nonspecific, with a high signal on T2-weighted images and a low signal on T1-weighted images [10]. In our patient, a mass with an isoechoic well-defined margin was observed on ultrasonography. Complete excision is an effective treatment for angioleiomyomas and lipoleiomyomas because recurrence or malignant transformations may occur. Moreover, posterior wall repair was performed with sutures because the weakening of the posterior wall after complete excision was concerned.
An inguinal mass should be included as a differential diagnosis in women presenting with inguinal swelling because rare tumors such as angioleiomyoma and lipoleiomyoma may occur in the inguinal canal. Laparoscopic excision with posterior wall repair may be an effective treatment of tumors in the inguinal canal.
Conflict of interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Compliance with ethical standards authorship declaration
This manuscript is not a duplicate publication and has been seen and approved by all authors.
Informed consent
Informed consent was obtained from all individual patients or their parents/guardians.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Ethical approval
This study followed the ethical guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Damsoyu Hospital: DSY-2017-012.



