-
PDF
- Split View
-
Views
-
Cite
Cite
Nikhil Aggarwal, Aman Bhargava, Appendiceal mucocele secondary to torsion in an asymptomatic patient, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz241, https://doi.org/10.1093/jscr/rjz241
Close - Share Icon Share
Abstract
Torsion of the appendix associated with an appendiceal mucocele is extremely rare with just a few published cases. To our knowledge, we report the first case of appendiceal mucocele secondary to torsion in an asymptomatic patient. In this case, numerous adhesions were found attaching the tip of the appendix mucocele to the peritoneum contributing to torsion as well as a lack of evidence for appendiceal neoplasm. Complications of appendiceal mucocele include obstruction, intussusception and pseudomyxoma peritonei, which has a particularly poor prognosis. Clinicians should, therefore, consider prompt surgical resection for definitive histopathological diagnosis and management.
INTRODUCTION
Mucocele of the appendix, a term first coined by Karl Freiherr von Rokitansky in 1842, describes an appendix that is grossly distended by mucus [1]. It is found in approximately 0.1–0.3% of appendectomy specimens and has non-specific symptomatology ranging from patients who are asymptomatic to having severe abdominal pain, often mimicking several common diseases [2, 3]. Mucocele formation is usually due to benign or malignant epithelial proliferation and less commonly due to inflammatory or obstructive causes. Torsion of the appendix associated with an appendiceal mucocele is extremely rare with just a few reported cases in the literature. To our knowledge, this is the first reported case of an appendiceal mucocele secondary to torsion in an asymptomatic patient.
CASE REPORT
An 80-year-old gentleman was referred to General Surgery by the Urology department following an incidental finding on a computerized tomography (CT) urogram, performed for investigation of haematuria, which self-resolved. The finding was of a well-circumscribed hypodense mass in the right iliac fossa measuring 5.2 × 4 cm. There was subtle focus of calcification at its wall with no communication with the urinary bladder (Figs 1 and 2).

Coronal view of CT showing a well-circumscribed hypodense mass in the right iliac fossa.

Transverse view of CT showing a well-circumscribed hypodense mass in the right iliac fossa.
The patient was asymptomatic from the mucocele. However, he had a past medical history of Crohn’s colitis, hypertension and benign prostatic hypertrophy.
The patient was discussed within a multi-disciplinary team (MDT) meeting and following which he underwent colonoscopy. This showed a small polyp in the sigmoid colon, no evidence of any pathology within the appendix orifice or within the caecum. Following MDT discussion, the patient was booked for laparoscopic right hemicolectomy with lymph node dissection in case of a malignant cause, such as mucinous cystadenocarcinoma.
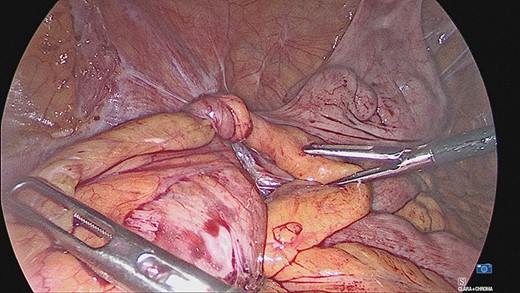
The appendiceal mucocele was visualised during the laparoscopic procedure. The adhesions surrounding the apex of the mucocele were released. There appeared to be volvulus of the appendix (Fig. 3). The main body of the appendix was normal with no evidence of malignancy seen during the surgery. On this basis, a right hemicolectomy was not performed. The appendix was amputated at the base and removed with the base tied (Fig. 4).
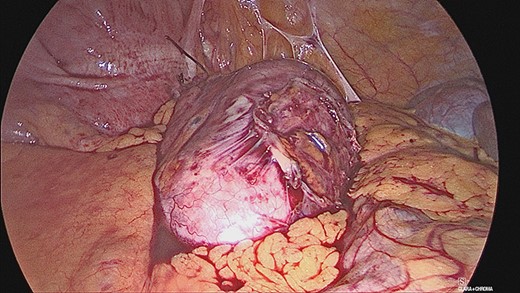
The patient was discharged from hospital the same day and followed up in clinic following histological analysis. Samples showed a grossly dilated appendix measuring 78 × 42 mm with a mesoappendix measuring up to 7 mm in thickness. Sections of the appendix revealed a thin wall with mucinous secretion in the lumen. There was complete replacement of epithelium lining by histiocytes with areas of multi-nucleated giant cell reaction. There was no evidence of any mucinous neoplasm.
DISCUSSION
Mucocele of the appendix refers to the dilation of the appendix with mucin accumulation [1]. The clinical presentation of mucoceles is usually vague, but most commonly presents with right lower quadrant pain. It is classified into four histologic types: retention mucinous cyst, mucosal hyperplasia, mucinous cystadenoma and mucinous cystadenocarcinoma. Complications of appendiceal mucocele include obstruction, intussusception and pseudomyxoma peritonei, which has a particularly poor prognosis with 5 and 10 year survival rates predicted at 50 and 10–30%, respectively. Therefore, prompt diagnosis and management is imperative, as discussed by Demetrashvili et al. [4, 5].
Torsion with an appendiceal mucocele is rare with only a few cases described in the literature. The mechanism of primary torsion remains unknown but is thought to be often associated with anatomical variations such as a narrow base, a long appendix or fan-shaped mesoappendix with consequent distal retention of mucus [6]. In this particular case, the mucocele was likely secondary to primary torsion given a lack of evidence for an appendiceal neoplasm both on histology and during surgery. Furthermore, adhesions attaching the tip of the appendiceal mucocele to the peritoneum are thought to have contributed to torsion. Torsion secondary to an appendiceal mucocele appears similar to torsion of the ovary, with the appendiceal mucocele twisting around its own axis with a short section of normal appendix connecting the cystic mass to the caecum acting as a fulcrum [7].
Given the rarity of the condition, pre-operative diagnosis of an appendiceal mucocele is difficult. An appendiceal diameter of 15 mm or more has been determined as the threshold for a diagnosis of appendiceal mucocele with a sensitivity of 83% and specificity of 92% [2]. CT enables evaluation of the extent of the disease and usually shows a round, cystic, tubular, hypoattenuated mass. Mural calcifications may be seen and are sensitive in the diagnosis of mucinous neoplasms [4].
Colonoscopy may reveal elevation of the appendiceal orifice with visible yellow mucous discharge as well as any synchronous or metachronous colon cancers [2]. Fine needle aspiration cytology is not recommended due to a risk of perforation and dissemination.
A right hemicolectomy is performed if malignancy is suspected based on imaging or intraoperative frozen section [2, 4]. In malignant cases, the risk of developing adenocarcinoma of the colon is greatly increased and therefore, follow-up and surveillance is recommended [8]. Furthermore, incidental appendiceal neuroendocrine tumours occur in 0.2–0.7% of surgical resections for suspected appendicitis. Although rare, these often require long-term follow-up [9].
In conclusion, we present the first reported case of primary torsion of the appendix resulting in an appendiceal mucocele in an asymptomatic patient. The presence of a round, cystic mass should alert clinicians at the possibility of an appendiceal mucocele. This case highlights that clinicians should consider primary torsion as a rare potential trigger of an appendiceal mucocele. Prompt surgical resection should be considered in all cases of appendiceal mucocele to achieve definitive histopathological diagnosis and management.
Conflict of Interest Statement
None declared.



