-
PDF
- Split View
-
Views
-
Cite
Cite
Sherif Monib, Mohamed Elkorety, Simon Thomson, A case of successful conservative management of gallstone ileus, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz253, https://doi.org/10.1093/jscr/rjz253
Close - Share Icon Share
Abstract
Gallstone ileus is an uncommon complication of cholelithiasis but an established cause of mechanical bowel obstruction in the elderly. Perforation of the small intestine proximal to the obstructing gallstone is rare, only a handful of cases having been reported. Management is mainly surgical, but conservative treatment is occasionally appropriate. We report the case of an 86-year-old female who presented with a clinical picture of bowel obstruction, proven to be related to gallstone ileus which resolved spontaneously. We discuss the role of conservative management for this condition.
INTRODUCTION
Gallstone ileus is a rare complication of gallstone disease with a variable and sometimes nonspecific clinical presentation. It requires a high index of suspicion, particularly in elderly patients presenting with signs of small bowel obstruction. In spite of the fact that management is mainly surgical, there is some room for conservative treatment in a selected group of patients. We report such a case and suggest guidelines for conservative management.
CASE REPORT
We are presenting a case of an 86-year-old female, who presented to Accident and Emergency department with a 4 day history of abdominal pain, distension and vomiting. There was no relevant past medical history apart from a recent episode of right upper quadrant pain, which had been investigated by abdominal ultrasound scan. This had shown sludge within the gallbladder lumen without calculi and diffuse thickening of the gall bladder wall suggesting acute cholecystitis.
General examination revealed dehydration. Vital signs revealed mild tachycardia with normal blood pressure, temperature and respiratory rate. Abdominal examination revealed mild abdominal distension with mild generalized tenderness mainly at the right upper quadrant and negative Murphy’s sign. Bowel sounds were present and digital rectal examination revealed an empty rectum.
Initial laboratory investigations revealed white blood cells 14.3 × 109/L, Hb 14.2 g/dL, platelets 402 × 109/L, PT 12.2 s, APTT 28.6 s, amylase 55 U/L, T. Bil 25 mg/dL, ALT 16 U/L, ALP 85 U/L, Alb 34 g/L, total calcium 2.42 mmol/L, urea 2.8 mmol/L, creatinine 47 umol/L, sodium 140 mmol/L and potassium 4.1 mmol/L.
Plain abdominal X-ray demonstrated a calcified lesion on the right as well as distended loops of small bowel (Fig. 1). Abdomino-pelvic contrast CT scan showed an abnormal gallbladder containing pockets of air and a fistulation through the lateral part of D2,with a 22 mm calcified lesion within the ascending colon (Fig. 2a–d). Based on the history, physical examination and CT scan findings, our diagnosis was of resolving gallstone ileus.
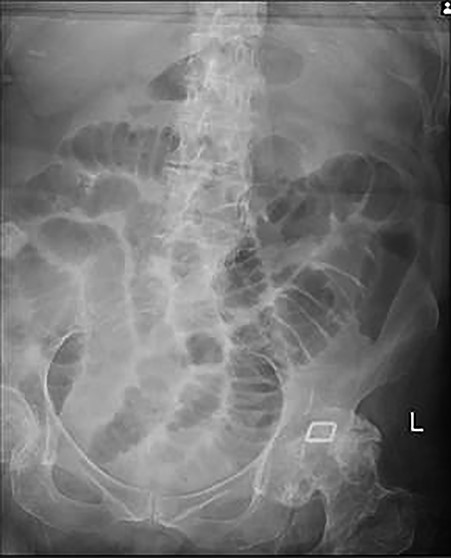
Plain abdominal X-ray at presentation demonstrating gallstone as well as distended loops of small bowel.

a,b,c,d: CT images scout, axial, coronal and sagittal planes, respectively demonstrating gallstone as well as distended loops of small bowel.
As the gallstone was seen within the ascending colon, the patient was managed conservatively for 2 days after which she was able to tolerate fluids then light diet. Follow-up abdominal X-ray revealed that the gallstone had reached the rectum with no radiological signs of bowel obstruction (Fig. 3). On the fourth day of admission, she opened her bowels and abdominal distension completely resolved.

Follow-up abdominal X-ray revealed the gallstone in the rectum and that bowel obstruction has now resolved.
She was seen in the outpatient department 6 weeks after her discharge with no symptoms, and we jointly agreed not to proceed with any further surgical intervention.
DISCUSSION
Gallstone “ileus” itself is a misnomer as the underlying pathology is that of mechanical obstruction of the bowel by a gallstone rather than a paralytic ileus as the name suggests. It was first described in 1654 by Dr. Erasmus Bartholin and is thought to be caused by impaction of a gallstone in the gastrointestinal tract after passing through a biliary-enteric fistula. Gallstone ileus is more common in women (the ratio being 3.5 females to 1 male) and older patients, particularly those older than 60 years. Other factors that contribute to gallstone ileus are a long history of cholelithiasis, repeated episodes of acute cholecystitis and stones greater than 2 cm. According to the literature, approximately 40–50% of patients eventually diagnosed with gallstone ileus have a history of recent bouts of biliary colic, jaundice or acute cholecystitis [1, 2].
Gallstone ileus is a rare complication of cholelithiasis and is one of the rarest forms of all mechanical bowel obstructions. In nonstrangulating mechanical small bowel obstruction, it accounts for 1–4% of causes and up to 25% in the elderly [3].
The diagnosis is often delayed since symptoms may be intermittent and investigations may fail to identify the cause of the obstruction. In 1941, Leo George Rigler described Rigler’s triad which is a combination of small bowel obstruction, gallstone outside the gallbladder and pneumobilia, as an aid to gallstone ileus diagnosis [4].
The principal goal in management of gallstone ileus is a quick effective relief of mechanical bowel obstruction. When appropriate, it is possible to avoid surgery. For example, if the stone is within the reach of an endoscope, either in the proximal small bowel or in the colon, there is the option to treat it by lithotripsy and removal of the fragments. Spontaneous passage of gallstones large enough to cause impaction has been reported, but most patients require surgical intervention and the prominent risk of perforation underlines why a conservative approach is rarely adopted [5]. Surgery is the treatment of choice, since spontaneous passage is uncommon especially when gallstone diameter is higher than 2.5 cm [6]. Surgical options include enterotomy (avoiding the inflamed site of impaction) with stone extraction alone, enterotomy and cholecystectomy with fistula closure, bowel resection alone and bowel resection with fistula closure [7].
In our case presentation, conservative treatment was supported by the CT showing the gallstone to have passed into the colon. If the gallstone is still in the ileum, we believe that initial conservative treatment may be a safe and effective option for patients with gallstones less than 25 mm in the absence of signs of bowel perforation or sepsis or of severe or worsening bowel obstruction. Such cases should be closely monitored by abdominal X-ray or CT to track movement of the gallstone and degree of obstruction.
Author’s contributions
ME and ST contributed in patient’s management. SM wrote the manuscript and did the literature review and ST edited the manuscript.
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
No ethical approval was needed for this case report.
Financial disclosure statement
There are no financial conflicts of interest to disclose.
Patient’s consent
Written informed consent was obtained from the patient to include images in the article.
Notes
This article has not been presented at any symposium or conference to date.



