-
PDF
- Split View
-
Views
-
Cite
Cite
Bogdan Toia, Jeremy J Ockrim, Tamsin J Greenwell, Ureteric reimplantation via vaginal route: a new surgical technique, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz235, https://doi.org/10.1093/jscr/rjz235
Close - Share Icon Share
Abstract
Vesicovaginal fistulae (VVF) and ureteric reimplantation are two rare complications of obstetric surgery. VVF can be repaired via a vaginal approach utilizing Martius fat pad interposition to minimize urethral complications and improve surgical outcomes, while ureteric reimplantation into the bladder classically necessitates an abdominal or laparoscopic approach. We present a new technique of ureteric reimplantation via vaginal approach with concomitant repair of a 5-cm VVF in a 25-year-old woman after an emergency caesarean section with bladder injury and ureteric transection. Good drainage was confirmed on MAG3 and successful vaginal birth (albeit preterm) was subsequently achieved.
INTRODUCTION
Bladder injury and ureteric transection are rare complications after an emergency caesarean section (C-section). If discovered intraoperatively, these injuries can be addressed to minimize complications such as vesicovaginal fistulae (VVF) formation or ureteric stricture [1].
This report describes a case of a VVF repair with Martius fat pad (MFP) interposition and concomitant reimplantation of strictured ureter via a vaginal approach.
CASE REPORT
A 25-year-old woman was referred from a secondary hospital following a major uterine rupture at 40 + 6 gestation resulting in stillbirth and bladder injury. She was expected to deliver by vaginal birth after caesarean as she already had one child that was delivered by straightforward C-section. Labour was induced at 40 weeks due to high blood pressure, but during this process, the patient reported a tearing sensation in her lower abdomen and was taken to theatre for an emergency C-section and was discovered to have a uterine rupture and intrauterine foetal death. The C-section resulted in bladder injury and right ureteric transection. Subsequently, she developed a residual vesicovaginal fistula associated with ureteric obstruction at the level of the repair, and required nephrostomy and indwelling catheter drainage (Figures 1 and 2).
She had vaginal VVF repair under our care. Intraoperatively, cystoscopy revealed a large oblique VVF extending over 5 cm with the right ureteric orifice not identifiable. Intraoperative nephrostogram suggested restricted drainage of contrast at the level of the right vesicoureteric junction. Via a vaginal approach, the distal ureteric orifice was circumscribed and the distal ureter mobilized. The ureteric stricture was then incised and the distal ureter resected, spatulated and reimplanted into the bladder. An anterograde guidewire was inserted through the nephrostomy into the bladder and a ureteric catheter placed over this wire to the renal pelvis. The fistula was closed with continuous polyglactin 910 3/0 suture in two layers, and modified Martius fat pad was mobilized on its posterolateral pedicle and sutured over the repair.
At a 1-year follow-up, the patient was complaining of flank pain, so an technetium-99m mercaptoacetyltriglycine renography (MAG3) was performed, showing good drainage but mild to moderate reflux into the reimplanted ureter. Normal bladder and sexual function were restored, and she was discharged from routine follow-up after 18 months. Following successful conception, she had a specialist obstetric review and was planned to have an elective C-section at between 37 and 38 weeks to avoid labour. Unfortunately, she had a premature vaginal delivery due to chorioamnionitis at 23 + 4 gestation complicated by sepsis with features of shock from which she and her baby made a full recovery (Figs. 1 and 2).
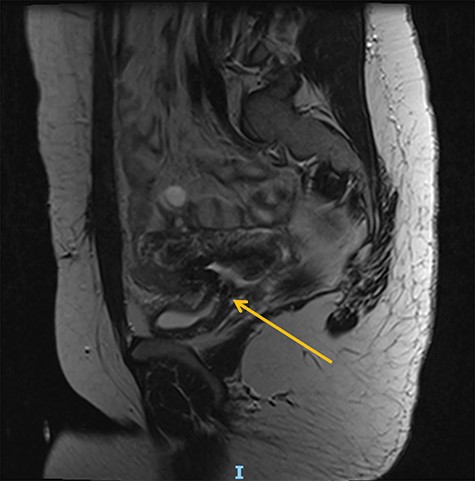
Preoperative magnetic resonance (MR) abdomen, sagittal plane. Arrow indicating vesicovaginal fistula
At the latest follow-up, 11 months after delivery (49 months postoperatively), she had no urinary symptoms of note and in particular none suggestive of fistula recurrence.
DISCUSSION
Ureteric injuries can occur in less than 1% of C-sections [1]. The medium- and long-term complications of these injuries are strictures which, even if located distally, would usually require further abdominal, laparoscopic or robot-assisted surgery to resect the strictured segment and reimplant the residual ureter into the bladder [2]. To our knowledge, a vaginal approach has never been described in literature.
Another complication of obstetric surgery is bladder injury, which could lead to the development of VVF. Multiple techniques have been described to repair iatrogenic fistulae, with the most noteworthy technique utilizing MFP interposition to provide a vascular pedicle to minimize urethral complications and improve outcomes in iatrogenic fistulae [3]. Patients undergoing repair are advised against vaginal delivery due to the risk of delivery-related fistula recurrence in up to 14% and other maternal and neonatal complications [4]. While these complications are reported after VVF repair in general, no specific literature data are available for delivery after VVF repair with MFP.
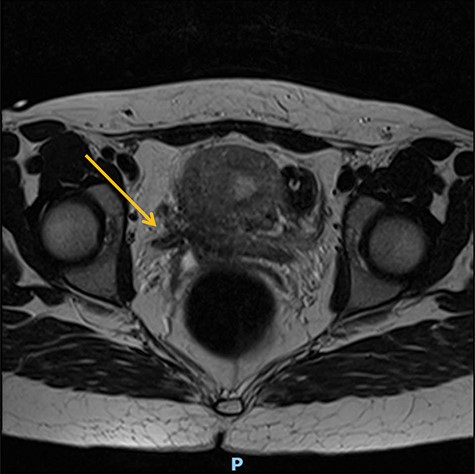
Preoperative MR abdomen, transverse plane. Arrow indicating obstructed right ureter
We utilized MFP interposition as previously described by Malde et al. [5]. The distally strictured was resected and successfully reimplanted into the bladder via the vaginal route at the same time as VVF repair with modified Martius fat pad (MFP) interposition.
This is the first report of ureteric reimplantation via a vaginal route as well as one of the few reported successful vaginal birth (albeit preterm) after VVF repair with MFP interposition.
Conflict of interest statement
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



