-
PDF
- Split View
-
Views
-
Cite
Cite
Ami P Patel, Dorsa Samsami, Chloe Lee, Asif Lakha, Eli D Ehrenpreis, The waiting game: laparoscopic repair of dual Morgagni and paraesophageal hernias in an elderly, infirm patient, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz225, https://doi.org/10.1093/jscr/rjz225
Close - Share Icon Share
Abstract
Morgagni hernias are congenital diaphragmatic disruptions that occur when intra-abdominal organs herniate posterior to the sternum. It is very rare to concomitantly diagnose a paraesophageal hernia (PEH) in a patient with a Morgagni hernia. Here, we describe an elderly female patient presenting with severe chest pain subsequently diagnosed with a non-strangulated Morgagni hernia as well as PEH. She underwent successful robotic laparoscopic surgical repair of the hernias with resolution of her symptoms. This case demonstrates the need for early surgical intervention of Morgagni hernias to prevent sequelae, such as strangulation, and the rising benefits of laparoscopic repairs in adult patients.
INTRODUCTION
Morgagni hernias are rarely encountered in elderly patients, as they are congenital diaphragmatic defects typically diagnosed at a young age, requiring early surgical repair [1]. Only 5–25% of congenital diaphragmatic hernias demonstrate late presentation [2]. Morgagni hernias occur when abdominal contents herniate through the sternocostal triangle, also known as the foramen of Morgagni [3]. If a Morgagni hernia remains asymptomatic, as 28% typically do in adults, it may not be diagnosed unless found incidentally [4, 5]. Immediate repair of Morgagni hernias is recommended and accepted as norm in order to avoid incarceration; however, surgery has been delayed or avoided in elderly or infirm patients [6]. One patient was followed for 18 years until surgical repair was required [7]. In other cases, patients eventually became symptomatic and needed surgical intervention [5]. Furthermore, concurrent PEH and Morgagni hernias remain very rare, with the first case reported by Lund et al. in 1958 [3].
A retrospective comparison of elective laparoscopic versus open surgical management of Morgagni hernias among 43 adult patients from 1987 to 2015 demonstrated no statistical significance in the complication rates; however, laparoscopically managed patients did experience shorter hospital stays. In a review of 269 cases of Morgagni hernia repairs, laparoscopic approaches were associated with lower 30-day mortality rates than laparotomies [8]. Laparotomies are the surgical method of choice in emergent situations [8]. In the past two decades, robotic laparoscopic surgeries have gained popularity secondary to decreased postoperative complication rates, shortened length of hospitalization and reduced morbidity [9, 10]. However, only one case of robotically repaired simultaneous PEH and Morgagni hernias has been described in the literature, thus a rare occurrence [1]. As per Fu et al., the patient tolerated the procedure well and suffered no postoperative complications, and no recurrence of symptoms was noted at a 3-month follow-up [1]. We present a case of an elderly patient with stage IV breast cancer, whose Morgagni hernia and PEH repair was delayed, but eventually she required surgery for intractable chest pain and risk of hernia strangulation or incarceration.
CASE REPORT
An 83-year-old female with a history of stage IV invasive ductal carcinoma of the right breast initially diagnosed at age 78, who was status post right modified radical mastectomy, and chemotherapy and radiation therapy directed at sacral bone metastasis, presented to the emergency department with chest pain. The patient had progressively worsening severe, squeezing substernal chest pain for 5 days, escalating from mild to severe pain. She had a known moderate-sized hiatal hernia reported via chest radiography 4 years prior with a history of mild, intermittent substernal chest pain unrelated to food intake that would resolve spontaneously. A computed tomography (CT) pulmonary angiogram with intravenous (IV) contrast performed 2 years prior for similar, but less intense, substernal chest pain demonstrated a non-strangulated Morgagni hernia and a large PEH. Surgical intervention was deferred due to spontaneous resolution of patient’s symptoms, no evidence of strangulation/incarceration and ongoing cancer-related therapies including denosumab, fulvestrant and ribociclib.
During the hospitalization, initial cardiac workup with 12-lead electrocardiogram and serial troponins was negative. The patient’s oncologic medications were held without improvement of the pain as well as to prevent leukopenia and neutropenia, if surgery was indicated. Palliative care was unable to achieve adequate pain control with oral and IV medications, and the patient did not want to pursue hospice care. Surgical consultation was obtained, and further evaluation with a CT scan of the chest, abdomen and pelvis with oral and IV contrast demonstrated an anteromedial diaphragmatic defect through which a prominent amount of mesenteric fat and a portion of the colon herniated representing a Morgagni hernia (Figs. 1–4). An increase in the size of the previously known PEH as well as the Morgagni hernia was noted. Due to continued chest pain unrelieved by opioids, a joint decision was made between surgeon, oncologist and the patient to proceed with surgery. She underwent successful robotic laparoscopic repair of the Morgagni hernia and PEH with dulex mesh for reinforcement. Her chest pain subsequently resolved. The patient gradually tolerated oral feeds and was eventually discharged in stable condition.

A sagittal view from the 2017 CT chest, abdomen and pelvis with IV and PO contrast demonstrates the Morgagni hernia with fat sweeping up through the diaphragmatic defect (red arrow) and a retrocardiac paraesophageal hernia (blue arrow).

A CT chest, abdomen and pelvis with PO and IV contrast in 2017 shows bowel gas with mesentery herniating anteriorly through a diaphragmatic defect, consistent with a Morgagni hernia (red arrow) that has increased in size since 2015.

The CT abdomen and pelvis with oral contrast from 2015 pictured above led to an initial diagnosis of a Morgagni hernia, identified by the red arrow.
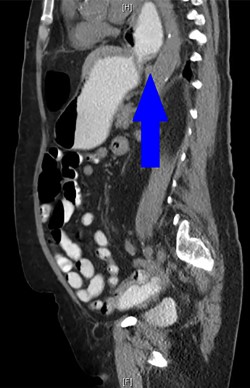
A CT abdomen and pelvis with oral contrast from 2015 demonstrates the presence of a PEH, identified by the blue arrow.
| Author . | Year . | Age (in years) . | Gender . | Symptoms . | Treatment . | Complications . | Postoperative hospitalization length . |
|---|---|---|---|---|---|---|---|
| Lund et al. | 1958 | 62 | Female | Chest pain | Laparotomy | None | Unknown |
| Ngage et al. | 2001 | 74 | Male | Respiratory distress | Laparotomy | None | 12 days |
| Cokmez et al. | 2002 | 65 | Female | Dyspnea, vomiting | Laparoscopy | None | 5 days |
| Eroglu et al. | 2003 | 67 | Male | Dyspnea, chest pain | Laparotomy | None | 5 days |
| Szentkereszty et al. | 2006 | 67 | Female | Epigastric pain, dysphagia | Laparoscopy | None | 7 days |
| Bettini et al. | 2015 | 76 | Male | Abdominal pain | Laparotomy | Pulmonary embolism, atrial fibrillation, Clostridium difficile colitis | 14 days |
| Zhou et al. | 2015 | 73 | Female | Chest pain, dyspnea | Laparoscopy | None | 7 days |
| Mittal et al. | 2018 | 71 | Male | Regurgitation, heartburn, vomiting | Laparoscopy | None | 8 days |
| Ozawa et al. | 2018 | 91 | Female | Vomiting | Laparoscopy | None | 30 days |
| Fu et al. | 2018 | 67 | Female | Dyspnea, chest pain, back pain, dysphagia, heartburn | Robotic-assisted laparoscopy | None | Unknown |
| Hassan et al. | 2019 | 53 | Female | Regurgitation, heartburn | Laparoscopy | None | 4 days |
| Our case | 2017 | 83 | Female | Chest pain | Robotic-assisted laparoscopy | None | 9 days |
| Author . | Year . | Age (in years) . | Gender . | Symptoms . | Treatment . | Complications . | Postoperative hospitalization length . |
|---|---|---|---|---|---|---|---|
| Lund et al. | 1958 | 62 | Female | Chest pain | Laparotomy | None | Unknown |
| Ngage et al. | 2001 | 74 | Male | Respiratory distress | Laparotomy | None | 12 days |
| Cokmez et al. | 2002 | 65 | Female | Dyspnea, vomiting | Laparoscopy | None | 5 days |
| Eroglu et al. | 2003 | 67 | Male | Dyspnea, chest pain | Laparotomy | None | 5 days |
| Szentkereszty et al. | 2006 | 67 | Female | Epigastric pain, dysphagia | Laparoscopy | None | 7 days |
| Bettini et al. | 2015 | 76 | Male | Abdominal pain | Laparotomy | Pulmonary embolism, atrial fibrillation, Clostridium difficile colitis | 14 days |
| Zhou et al. | 2015 | 73 | Female | Chest pain, dyspnea | Laparoscopy | None | 7 days |
| Mittal et al. | 2018 | 71 | Male | Regurgitation, heartburn, vomiting | Laparoscopy | None | 8 days |
| Ozawa et al. | 2018 | 91 | Female | Vomiting | Laparoscopy | None | 30 days |
| Fu et al. | 2018 | 67 | Female | Dyspnea, chest pain, back pain, dysphagia, heartburn | Robotic-assisted laparoscopy | None | Unknown |
| Hassan et al. | 2019 | 53 | Female | Regurgitation, heartburn | Laparoscopy | None | 4 days |
| Our case | 2017 | 83 | Female | Chest pain | Robotic-assisted laparoscopy | None | 9 days |
| Author . | Year . | Age (in years) . | Gender . | Symptoms . | Treatment . | Complications . | Postoperative hospitalization length . |
|---|---|---|---|---|---|---|---|
| Lund et al. | 1958 | 62 | Female | Chest pain | Laparotomy | None | Unknown |
| Ngage et al. | 2001 | 74 | Male | Respiratory distress | Laparotomy | None | 12 days |
| Cokmez et al. | 2002 | 65 | Female | Dyspnea, vomiting | Laparoscopy | None | 5 days |
| Eroglu et al. | 2003 | 67 | Male | Dyspnea, chest pain | Laparotomy | None | 5 days |
| Szentkereszty et al. | 2006 | 67 | Female | Epigastric pain, dysphagia | Laparoscopy | None | 7 days |
| Bettini et al. | 2015 | 76 | Male | Abdominal pain | Laparotomy | Pulmonary embolism, atrial fibrillation, Clostridium difficile colitis | 14 days |
| Zhou et al. | 2015 | 73 | Female | Chest pain, dyspnea | Laparoscopy | None | 7 days |
| Mittal et al. | 2018 | 71 | Male | Regurgitation, heartburn, vomiting | Laparoscopy | None | 8 days |
| Ozawa et al. | 2018 | 91 | Female | Vomiting | Laparoscopy | None | 30 days |
| Fu et al. | 2018 | 67 | Female | Dyspnea, chest pain, back pain, dysphagia, heartburn | Robotic-assisted laparoscopy | None | Unknown |
| Hassan et al. | 2019 | 53 | Female | Regurgitation, heartburn | Laparoscopy | None | 4 days |
| Our case | 2017 | 83 | Female | Chest pain | Robotic-assisted laparoscopy | None | 9 days |
| Author . | Year . | Age (in years) . | Gender . | Symptoms . | Treatment . | Complications . | Postoperative hospitalization length . |
|---|---|---|---|---|---|---|---|
| Lund et al. | 1958 | 62 | Female | Chest pain | Laparotomy | None | Unknown |
| Ngage et al. | 2001 | 74 | Male | Respiratory distress | Laparotomy | None | 12 days |
| Cokmez et al. | 2002 | 65 | Female | Dyspnea, vomiting | Laparoscopy | None | 5 days |
| Eroglu et al. | 2003 | 67 | Male | Dyspnea, chest pain | Laparotomy | None | 5 days |
| Szentkereszty et al. | 2006 | 67 | Female | Epigastric pain, dysphagia | Laparoscopy | None | 7 days |
| Bettini et al. | 2015 | 76 | Male | Abdominal pain | Laparotomy | Pulmonary embolism, atrial fibrillation, Clostridium difficile colitis | 14 days |
| Zhou et al. | 2015 | 73 | Female | Chest pain, dyspnea | Laparoscopy | None | 7 days |
| Mittal et al. | 2018 | 71 | Male | Regurgitation, heartburn, vomiting | Laparoscopy | None | 8 days |
| Ozawa et al. | 2018 | 91 | Female | Vomiting | Laparoscopy | None | 30 days |
| Fu et al. | 2018 | 67 | Female | Dyspnea, chest pain, back pain, dysphagia, heartburn | Robotic-assisted laparoscopy | None | Unknown |
| Hassan et al. | 2019 | 53 | Female | Regurgitation, heartburn | Laparoscopy | None | 4 days |
| Our case | 2017 | 83 | Female | Chest pain | Robotic-assisted laparoscopy | None | 9 days |
DISCUSSION
While Morgagni hernias are rare, simultaneously occurring Morgagni and paraesophageal hernias are even rarer, as only 11 cases have been reported since 1958 (Table 1) [5]. Patients presented with chest pain in 33% of the previously reported cases. Others presenting symptoms include dyspnea, vomiting, dysphagia, respiratory distress and abdominal pain [5]. Surgical repair of Morgagni hernias is recommended to prevent strangulation or for symptom relief. Patients with coexisting PEH and Morgagni hernias were treated laparoscopically in the previous 7 out of 11 cases [5].
Our case demonstrates the feasibility and success of utilizing robotic laparoscopic hernia repair in the setting of a very rare presentation of concurrent Morgagni hernia and PEH in an elderly patient. The majority of surgeons agree that watchful waiting of Morgagni hernias should not be employed secondary to risk of complications secondary to strangulation or incarceration [6]. Previously, it was common to repair Morgagni hernias in adults with transabdominal and transthoracic techniques. However, the transabdominal approach, which is favored by surgeons due to ease of accessibility to abdominal viscera, is favored in patients with peritonitis for better outcomes [5].
This case is only the second report of a concurrent Morgagni hernia and PEH repair utilizing robotic technology (Table 1) [1]. A literature review reveals that laparoscopic repair of uncomplicated Morgagni hernias is associated with decreased postoperative hospitalization length and fewer postoperative complications [8, 9]. A review of 298 Morgagni hernia repairs reports little morbidity or mortality (0% 30-day mortality of patients undergoing laparoscopic repair versus 4% undergoing laparotomy) associated with modern techniques such as laparoscopic repair [8]. Laparoscopic repair of dual Morgagni hernia and PEH can be performed in elderly patients with low rates of intraoperative and postoperative complications, decreased morbidity postoperatively and shortened postoperative stays [10]. Our cases suggest that elective performance of laparoscopic repair of complex hernias should be considered, even in poor surgical candidates, to prevent complications requiring emergent or emergency procedures.
Conflict of interest statement
No funding was received. No conflicts to declare.



