-
PDF
- Split View
-
Views
-
Cite
Cite
Yazan N AlJamal, Jacob J Billings, Eric J Dozios, A black esophagus as a result of treatment of inferior vena cava occlusion by a massive pelvic schwannoma, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz237, https://doi.org/10.1093/jscr/rjz237
Close - Share Icon Share
Abstract
This case presentation involves a 57-year-old-male who suffered multiple adverse sequels from the delayed diagnosis of a large presacral mass. He initially presented with lower extremity deep vein thrombosis (DVT). Several months later, he had developed a pulmonary embolus. Imaging demonstrated a 13 × 14 cm presacral pelvic mass that occluded the right-sided venous return from the leg and caused the DVT and pulmonary embolism. An inferior vena cava filter was placed and eventually clotted. He then was referred to our institution for surgical consultation. The patient received lytic therapy and unfortunately developed hematemesis and a significant hemoglobin drop. An esophagogastroduodenoscopy (EGD) showed a black esophagus. A transthoracic echocardiogram showed a patent foramen ovale. The patient eventually stabilized and a repeat EGD a week later showed resolution of the ischemic esophagus. The patient later underwent a resection of the pelvic mass. The surgical approach and the surgical decision-making will be discussed.
INTRODUCTION
Black esophagus or acute esophageal necrosis (AEN) is a rare condition seen in critically ill patients [1]. It presents with a darkened esophagus caused by hematemesis and melena. It affects 0.0125–0.2% of patients while having esophagogastroduodenoscopy (EGD). Under endoscopy, it looks black and shows signs of necrosis, most commonly in the distal portions of the esophagus. The histopathology shows necrotic debris with mucosal and submucosal necrosis. AEN arises in the setting of multiorgan dysfunction, traumatic transection of the thoracic aorta, thromboembolic phenomena, malignancy, etc. [1, 2].
CASE
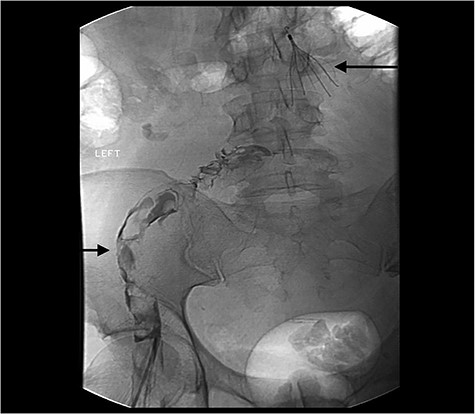
This case presentation involves a 57-year-old male who suffered multiple adverse sequela form the delayed diagnosis of a large presacral mass. He initially presented with left lower extremity deep venous thrombosis (DVT). Several months later, he developed a pulmonary embolus (PE). Due to his complaints of right groin pain, imaging was obtained that demonstrated a 13 × 14 cm presacral pelvic mass, which turned out to be a schwannoma on biopsy (Fig. 1). The presacral mass occluded the right-sided venous return from the leg and caused the DVT (Fig. 2) and PE. Due to the extensive DVT and PE, the patient had an inferior vena cava (IVC) filter that was placed and eventually clotted. He then was referred to our institution for surgical consultation.

Axial view of CT abdomen and pelvis shows a 13 × 14 cm presacral pelvic mass.
After the case was discussed with multiple teams and deemed too unsafe for surgery, the patient was admitted to the intensive care unit, bilateral thrombolytic catheters were placed from the legs to above the IVC, and he was treated with intravascular thrombolytic (Alteplase and Heparin) therapy (Fig. 3). On Day 5, he developed bloody emesis and was noted to have a hemoglobin drop from 12 to 8 g despite blood transfusions. The patient was resuscitated, and an EGD demonstrated a blackened esophagus of the entire esophagus with no involvement into the stomach (Fig. 4). Considering these findings, transthoracic echocardiogram (TTE) and chest computed tomography (CT) angiogram (CTA) were performed, which revealed patent foramen ovale (PFO) with small right to left shunt and an edematous esophagus and duodenum with no perforation or arterial inflow problem, respectively. No intervention was performed. The patient eventually stabilized and a repeat EGD a week later showed resolution of the ischemic esophagus. Patient was started back on liquid diet, which was advanced to solid diet and was discharged a week later.
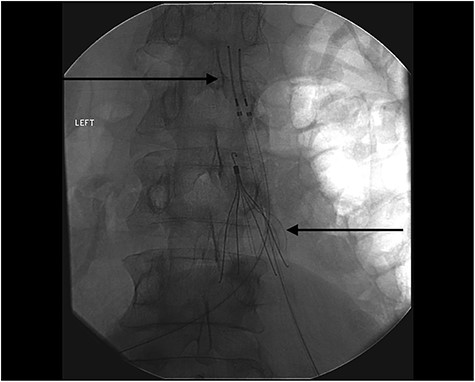
IVC filter and bilateral intravascular catheters to administer thrombolytic (Alteplase and Heparin) therapy. The upper left corner shows the Thrombolytic Catheter and the right lower arrow shows that IVC filter.
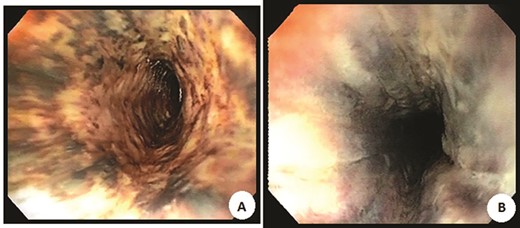
Endoscopic images of the proximal (A) and distal (B) black esophagus.
Two months later, the patient was taken to the operating room for resection of the pelvic mass. The tumor was mobilized and broken into four quadrants to be excised separately (Fig. 5). Each quadrant was mobilized and excised before being reconstructed on the back table. It was very solid and non-vascular.
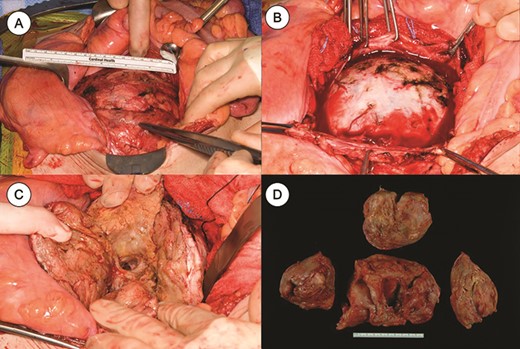
A large pelvic mass was exposed (A, B), and removed carefully through pieces (C, D).
The patient had uneventful course postoperatively and anticoagulation was continued for 8 months. He has not had any recurrence of lower extremity swelling or chest pain or dyspnea.
DISCUSSION
AEN ‘black esophagus’ is a rare life-threatening condition characterized by circumferential black appearing friable esophageal mucosa involving various length of the esophagus [1, 3]. Most commonly is affecting the distal esophagus, however few cases reported proximal esophagus [3]. Endoscopic appearance is diagnostic, and biopsies are not necessary unless if infectious causes are suspicious. The pattern of insult is unique ‘inside out’ and may involve full thickness of the esophagus, so close monitoring is the key.
In this case, we have described a unique presentation of black esophagus few days after the patient did receive intravascular thrombolytic. Patient developed hematemesis, dizziness and hypotension. Multiple studies have shown a combination of multiple factors behind the development of the black esophagus. Our patient underwent EGD, which revealed a necrotic mucosa circumferentially from just below the upper esophageal sphincter stopping exactly at the GE junction. The stomach was completely normal. It was felt that this may be ischemic in etiology. A TTE showed PFO with a small right to left shunting. CTA of the chest revealed thickened and edematous esophagus. The similar findings are thicken and edematous duodenum from the CTA. No obvious etiology could be identified. The question being asked is whether he has had embolization into the esophageal arterial supply. This would be extremely unusual, particularly given that there is some duodenal involvement as well. Intra-arterial thrombosis of the esophageal vessels in the setting of PFO with thrombolytic therapy could be considered. To date, there are no known treatments for black esophagus. The current recommendation is to intensively treat the patient’s comorbidities, optimize vascular perfusion, aggressively suppress acid production and treat esophageal infections, if present [3, 4]. The overall mortality in the largest case review to date was 32%. The high mortality was most frequently secondary to the seriousness of comorbid disease states. The mortality secondary to esophageal disease alone was 6% [1, 3].
Despite of the rough perioperative course, the intraoperative surgical planning was challenging. Pelvic neurogenic tumors had a high local recurrence rate and an aggressive approach, by an experienced multidisciplinary team who can achieve tumor-free resections, should improve outcome [5, 6].
Funding
There was no external funding.
Conflict of interest statement
None declared.
REFERENCES
- deep vein thrombosis
- pulmonary embolism
- ischemia
- consultation
- vena cava filters
- leg deep vein thrombosis
- patent foramen ovale
- upper gastrointestinal endoscopy
- hematemesis
- hemoglobin
- decision making
- neurilemmoma
- surgical procedures, operative
- diagnostic imaging
- esophagus
- leg
- pelvis
- pelvic mass
- echocardiography, transthoracic
- inferior vena cava syndrome
- venous return
- delayed diagnosis



