-
PDF
- Split View
-
Views
-
Cite
Cite
Michael Iannamorelli, Adam Bowling, Elie Semaan, Eroded GDA coil surgically managed with Roux-en-Y reconstruction, Journal of Surgical Case Reports, Volume 2019, Issue 8, August 2019, rjz234, https://doi.org/10.1093/jscr/rjz234
Close - Share Icon Share
Abstract
Here, we describe the case of a 56-year-old African American male who initially presented to the emergency department with 2 days of abdominal cramping, epigastric pain, loss of consciousness, melena and hematochezia. He underwent coil embolization of his gastroduodenal artery by the interventional radiology team after it was felt he was a high risk for rebleed. The patient then returned to the hospital with 3 weeks of epigastric pain, lightheadedness and melanotic stool. An upper endoscopy revealed a metallic coil embedded into the duodenal bulb. This coil was believed to be from prior embolization to the gastroduodenal artery. The patient then underwent a laparoscopic distal gastrectomy and partial duodenectomy with antecolic antegastric Roux-en-Y reconstruction bypassing the area where erosion occurred.
INTRODUCTION
Approximately 90–95% of upper gastrointestinal (GI) bleeding can be controlled with a therapeutic endoscopy. The remaining 5–10% of cases ultimately require either an emergency operation or endovascular embolization [1]. Successful rates of embolization are shown to be 51–94% [2]. Known risks of embolization include migration to terminal vascular beds causing organ ischemia, pseudoaneurysm formation, embolic events and, rarely, coil migration [3]. Here, we present a 56-year-old male who presents over 3 years after the embolization of his gastroduodenal artery (GDA) with a coil eroded into his duodenum causing GI bleeding.
CASE REPORT
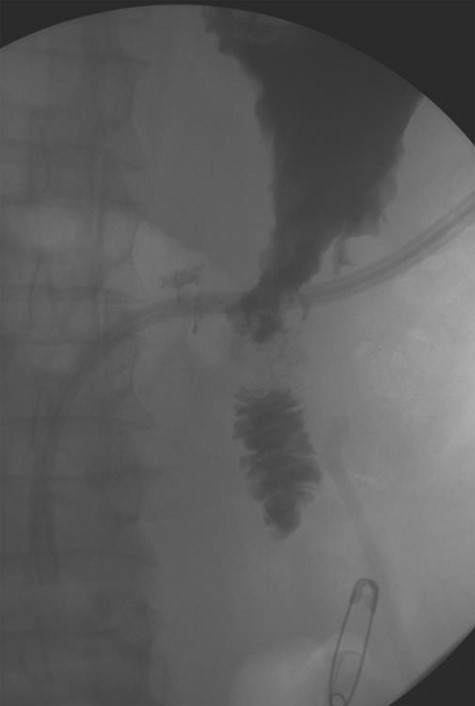
A 56-year-old African American male presented in 2015 with abdominal pain, with associated melena and hematochezia. The patient has a history of chronic back pain for which he takes 600 mg ibuprofen daily, alcohol abuse, tobacco use and a previous GI bleed in 2011, which necessitated 6 units (U) of packed red blood cells (PRBCs) and emergency therapeutic endoscopy. The patient was found to be hypotensive to 76/56 mm Hg, and hemoglobin (Hgb) was found to be 9.4 g/dl, from a previous baseline of 10.6 g/dl. His rectal examination was guaiac positive. A repeat Hgb was found to be 6.5 g/dl. The patient was given 3 U of PRBC and an emergency endoscopy was performed. On endoscopy, the patient was found to have a 6 cm gastric ulcer with an associated vessel underneath of a large clot. Due to the high risk nature of the bleed, it was felt by the gastroenterologist that the patient should undergo an endovascular angioembolization (Fig. 1). The patient was brought to the Interventional Radiology Suite for the procedure. The patient’s right common femoral artery was accessed and the celiac trunk was selected. A subselective common hepatic arteriogram was performed, which demonstrated active extravasation arising from the proximal aspect of the GDA. The GDA was then coil embolized both proximal and distal to the site of bleeding using five microcoils. Repeat arteriogram demonstrated no further opacification of the GDA and no further extravasation (Fig. 2).
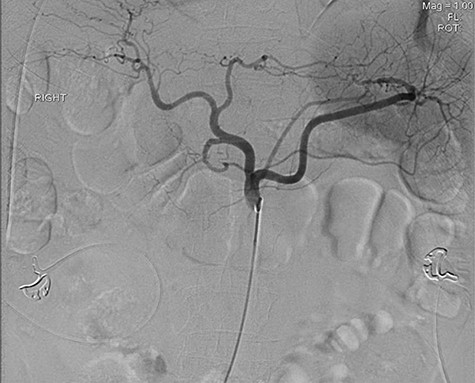
Demonstrating active extravasation of the GDA during a subselective GDA arteriogram

Demonstrating coil embolization of the GDA with no opacification


Single axial view of subsequent computed tomography scan demonstrating scattering from GDA coil with associated area suspicious for ulcer in duodenal bulb
The patient was discharged 5 days later with acid suppression medications.
Three years later, the patient presented to the emergency department with epigastric pain as well as melena. The patient could not remember the last time he took any acid suppression medication. He had increased his intake of ibuprofen. The patient was found to have a Hgb of 6.5 g/dl. He was given 2 U of PRBC and was taken to the endoscopy suite by the gastroenterology team. The endoscopy demonstrated a posterior duodenal bulb ulcer with a metallic ring in the center (Fig. 3). At this point, the general surgery team was consulted. A computed tomography scan of his abdomen and pelvis was obtained to further guide our operative decision-making (Fig. 4).
A laparoscopic distal gastrectomy and partial duodenectomy with antecolic antegastric Roux-en-Y reconstruction with a pancreaticobiliary limb of 50 cm and the Roux limb of 50 cm and esophagogastroduodenoscopy were performed. As the patient had been positive for Helicobacter pylori on endoscopic biopsy and there was increased concern for his use of alcohol as well as his living situation, a definitive acid suppression operation was also performed. The pathology returned as chronic gastritis with associated ulcer with mild metaplasia, the H. pylori on immunohistochemistry was positive. The patient on postoperative day (POD) 1 had a swallow study, which demonstrated a patent gastrojejunostomy with adequate flow distally (Fig. 5). On POD 5 the patient was discharged on a proton pump inhibitor and treatment for his H. pylori.
DISCUSSION
This case illustrates a patient who underwent endovascular embolization of his GDA for recurrent upper GI bleeding. The patient returned over 3 years later and was found to have a coil that had eroded into his duodenal bulb. The patient underwent a laparoscopic partial gastrectomy and partial duodenectomy with Roux-en-Y reconstruction. This case illustrates a novel idea in the treatment of patients who have had previous coil embolizations that have eroded, but are also at high risk for recurrent ulcerations. There are case reports discussing the erosion of a coil from a GDA embolization, but few have gone further to discuss the definitive operation in a patient with multiple medical and social variables. We decided to perform a Roux-en-Y bypass as to allow the ulcerated segment of the duodenum to heal and to definitively address the issue of acid production. There are alternatives such as a truncal vagotomy with pyloroplasty, but this technique would not address the issue of allowing the ulcerated area to heal, and a duodenotomy and coil extraction would prove to be a difficult and high-risk operation.
Approximately 5–10% of all nonvariceal upper GI bleeds will require further intervention from endoscopic therapies [1]. Also, 5–10% of upper GI bleeds are associated with mortality, due to advanced age, patient’s other comorbidities or associations with large transfusion requirements [4]. Open operations have become reserved for those patients in which endovascular therapy is not amenable or those with a bleed that is difficult to locate [5]. It is stated that the left gastric and the GDA supply 80–90% of upper GI bleeds [6]. There are sites that are proponents of ‘empiric’ embolization that using these methods have decreased the rate of recurrent bleeding as well as need for additional procedures [6]. There have been multiple case reports demonstrating the ability of coils to migrate into the small bowel causing obstructive symptoms, eroding into the biliary tract and the stomach, but this is when looking at visceral artery pseudoaneurysms.
This case demonstrates the ability to use endovascular embolizations for a high risk of rebleeding gastric ulcer. This also demonstrated that these interventions are not with risk, however. The GDA coil eroded into the first portion of the duodenum and was associated with an infection with H. pylori. This lead to the patient requiring not only an operation bypassing the area of the duodenum where the coil had eroded into but also a definitive acid suppression surgery as well. This case can help aid the future planning of managing patients with an acute GI bleed from coil embolizations.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- epigastric pain
- upper gastrointestinal endoscopy
- embolization
- hematochezia
- roux-en-y anastomosis
- emergency service, hospital
- feces
- laparoscopy
- melena
- interventional radiology
- reconstructive surgical procedures
- unconsciousness
- duodenal bulb
- lightheadedness
- billroth i procedure
- gastroduodenal artery
- african american
- erosion
- abdominal cramps
- duodenectomy



