-
PDF
- Split View
-
Views
-
Cite
Cite
Kunitaka Kuramoto, Osamu Nakahara, Yuto Maeda, Sayahito Kumamoto, Akira Tsuji, Shintaro Hayashida, Yuki Oya, Hidekatsu Shibata, Masayoshi Iizaka, Shinjiro Tomiyasu, Hironori Hayashi, Yukihiro Inomata, Hideo Baba, Single incision laparoscopic surgery (SILS) for Meckel’s diverticulum, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz210, https://doi.org/10.1093/jscr/rjz210
Close - Share Icon Share
Abstract
A 65-year-old male patient presented with a chief complaint of abdominal pain. Abdominal computed tomography (CT) showed slight intestinal dilation and obstruction of the upper right quadrant of the small intestine, while ectopic gastric mucosal scintigraphy revealed abnormal accumulation in agreement with the CT-identified structure. The cause of bowel obstruction was diagnosed as Meckel’s diverticulum; the patient was referred for surgery. A small laparotomy was performed with a 35-mm skin incision to the center of the navel. Once a lap disk was attached, a laparoscope was inserted to visualize the abdominal cavity. The small intestine that includes the structure was pulled out from the umbilicus to the outside of the peritoneal cavity and partially resected. On the pathological tissue findings, the patient was diagnosed with Meckel’s diverticulum. We report our experience with single-lap laparoscopic surgery for a case of intestinal obstruction caused by Meckel’s diverticulum and review pertinent literature.
INTRODUCTION
Due to advances in equipment and technology, the applications of laparoscopic surgery continue to expand [1]. Especially, an intraperitoneal examination is advantageous when preoperative diagnosis is difficult and treatment has to be continued [1, 2]. Depending on the disease, reduced-port laparoscopic surgery may be considered as an option.
Here, we report our experience with single incision laparoscopic surgery (SILS) for a case of intestinal obstruction caused by Meckel’s diverticulum and review the pertinent literature.
CASE REPORT
A 65-year-old male patient presented with a chief complaint of abdominal pain. He had a history of skin transplantation due to burns, and no significant family or occupational history. The patient’s current medical history included emesis and a heightened emotional state the day before presentation to the Emergency Department. On admission, all vital signs were stable. Abdominal findings were abdominal fullness by palpation, but no myopathic defense.
Abdominal computed tomography (CT) showed slight intestinal dilation (Fig. 1a). No abnormal findings were noted on blood biochemical analysis, other than the white blood cell count, C reactive protein levels, and a mild inflammatory response. On admission, a diagnosis of bowel obstruction was made. CT at the time of diagnosis showed an obstruction of the upper right quadrant of the small intestine (Fig. 1a), while ectopic gastric mucosal scintigraphy revealed abnormal accumulation in agreement with the structure identified by CT (Fig. 1b).
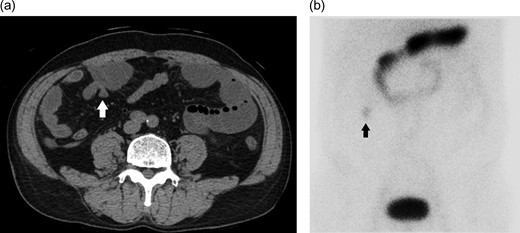
a) A structure that becomes small blind and has blind end so that it protrudes from the small intestine (white arrow). (b) Accumulation in the area close to the structure pointed out by scintigraphy (black arrow).
The cause of bowel obstruction was diagnosed as Meckel’s diverticulum; thus, the patient was referred for surgery.
A small laparotomy was performed by a skin incision of 35-mm length to the center of the navel (Fig. 2a). Once a lap disk was attached, a laparoscope was inserted to visualize the abdominal cavity. In the right upper quadrant, a structure was identified that protruded from the small intestine approximately 130 cm from the end of the ileum and became a blind end (Fig. 2b), which was pulled out from the umbilicus to the outside of the peritoneal cavity. The small intestine that includes the structure was partially resected. The postoperative course was good.
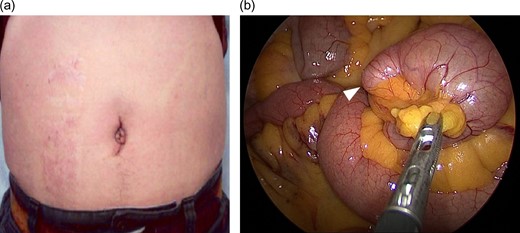
(a) 35 mm incision in the navel. (b) Accept a structure that is blinded to protrude from the small intestine (arrow head).
In the small intestine, a diverticulum protruding like a bag out of the wall of approximately 40 × 15 mm was observed (Fig. 3a). A diverticulum has the basic structure of the mucosa to muscle layer. In this case, most of the diverticulum mucosa was composed of gastric fundus glandular mucosa, while no pancreatic tissue was observed (Fig. 3b). On the basis of these findings, the patient was diagnosed with Meckel’s diverticulum.
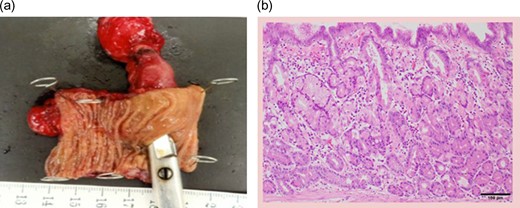
(a) Partial resection of the small intestine (diverticula length is approximately 45 mm). (b) Diverticulum mucosa composed of gastric fundus glandular mucosa.
DISCUSSION
As originally described by Fabricius Hidanus in 1598, Meckel’s diverticulum was named in honor of Johann Friedrich Meckel who illustrated its embryological origin in 1809 [3, 4]. Meckel’s diverticulum is a relatively common congenital gastrointestinal malformation left behind by the egg yolk duct during the embryonic period with a frequency of about 2–3% of the general population [2]. In adults, Meckel’s diverticulum exists on the sides of the mesenteric membrane with an attachment of approximately 60–130 cm from the oral cavity than the ileocecal valve [1].
Meckel’s diverticulum is rarely diagnosed because most cases remain asymptomatic. Moreover, symptoms accompanying Meckel’s diverticulum, which include hemorrhage, intestinal obstruction, intussusception, perforation, and diverticulitis, emerge less commonly with age, and more than 70% of symptomatic patients are under the age of 20 years [2, 5]. Accordingly, intestinal obstruction due to Meckel’s diverticulum in adults, as seen in the present case, is a relatively rare disease. Multidetector-row CT (MDCT) has been considered useful for diagnosis of Meckel’s diverticulum [6, 7]. It was used for diagnosis in the present case as well; the added availability of coronal-section and sagittal-section images allowed to depict a cystic shadow that appeared to be continuous with the small intestine and ended at the blind extremity, and was useful to diagnose the presence.
Capsule endoscopy and double-balloon endoscopy of the small intestine have recently been reported to be useful for diagnosis of Meckel’s diverticulum, and can be bridging tools in treatment, such as evaluation from the lumen of the digestive tract and lesion marking; however, these are presently available only in a limited number of institutions [8]. In general, scintigraphy using radionuclides is considered to be unsuitable for emergency examinations because it takes time to obtain the required radionuclide and perform a test; however, scintigraphy was a useful supplementary diagnostic method for Meckel’s diverticulum in the present case because 99mTc was readily available at our hospital and the examination could be performed in a relatively short period of time [7].
Laparoscopic surgery is widely used as a surgical treatment for abdominal diseases [8]. Recently, single-incision laparoscopic surgery has been reported as an even less invasive procedure and is also indicated for diverse conditions [9]. However, it has some technical limitations; for example, counter-traction by an assistant is not possible because only two forceps by the surgeon can be used at a time, and surgical manipulations are limited because of the interference with the forceps and scope [10]. In single-incision laparoscopic surgery for small intestinal diseases, it is also possible to guide the lesion site to the outside of the body, observe the entire small intestine, and resect and reconstruct the small intestine. Unlike in the conventional multiport laparoscopic surgery, extension of the incision or creation of additional incisions is not required in single-incision laparoscopic surgery because of the availability of the umbilical port hole. Single-incision laparoscopic surgery is comparable to conventional open surgery in terms of surgical results (operation time, blood loss, duration of hospital stay, and incidence of complications), and has an esthetic advantage. Single-incision laparoscopic surgery appears to be a useful procedure to consider when CT and scintigraphy suggest a lesion in the small intestine due to Meckel’s diverticulum, as seen in the present case, because radical surgery can be directly performed after definitive diagnosis by staging laparoscopy.
In conclusion, we could perform SILS as the curative surgery for Meckel’s diverticulum which was suspected preoperatively by scintigraphy. SILS for the Meckel’s diverticulum is considered to be a useful operative method for achieving radical cure and providing a cosmetic merit.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLOSURE
The authors have no conflicts of interest to declare.
REFERENCES
- radionuclide imaging
- abdominal pain
- dilatation, pathologic
- intestinal obstruction
- intestine, small
- intestines
- laparoscopes
- laparotomy
- greater sac of peritoneum
- surgical procedures, operative
- umbilicus
- meckel's diverticulum
- mucous membrane
- skin
- surgery specialty
- laparoscopic surgery
- abdominal ct
- Abdominal cavity
- chief complaint



