-
PDF
- Split View
-
Views
-
Cite
Cite
Kyle A Andrews, Marshall Gillette, Ronit V Shah, Lucas A Mckean, Christopher G Sanford, Type IV tibial tubercle fracture—Salter–Harris type II variant, Journal of Surgical Case Reports, Volume 2019, Issue 7, July 2019, rjz209, https://doi.org/10.1093/jscr/rjz209
Close - Share Icon Share
Abstract
Fractures about the tibial tubercle are uncommon fracture patterns, seen most often in adolescent males as they approach skeletal maturity. Compartment syndrome has a high association with these fractures requiring close monitoring, and a heightened level of suspicion. Tibial tubercle fractures are typically stratified using the Ogden classification. The type of intra-articular involvement and degree of displacement guide appropriate treatment. This report highlights a 14-year-old male patient who suffered a type IV tibial tubercle fracture with a unique Salter–Harris II, or transitional, component posteriorly that was unable to be closed reduced and developed compartment syndrome. He underwent fasciotomy, open reduction, and temporary external fixation. Once the status of the soft tissues improved, he underwent staged open reduction and internal fixation with skin grafting. The patient’s fracture and soft tissues healed and he currently ambulates without assistance or pain, and has returned to all desired activities including competitive sports.
INTRODUCTION
Tibial tubercle fractures constitute < 1% of all physeal fractures and 3% of proximal tibial fractures [1]. These injuries are most commonly seen in adolescent males approaching skeletal maturity. The proximal tibial physis closes from posterior to anterior and from proximal to distal; this places the tibial tubercle apophysis at increased risk of fracture in this age group [2]. This closure pattern also makes transitional fractures about the proximal tibia possible. The fracture is almost exclusively seen in males and is thought to be the result of a violent contraction of the quadriceps which can occur with jumping or forced knee flexion against a contracted quadriceps muscle [3]. In nondisplaced or minimally displaced type I tibial tubercle fractures, management with casting alone may be sufficient. However, displaced type I fractures and most other patterns often require open reduction and internal fixation. Compartment syndrome is notoriously associated with tibial tubercle fractures due to proximity of the fracture to the recurrent anterior tibial artery; therefore, close monitoring is paramount even in nondisplaced fracture patterns [4, 5].
We present a 14-year-old male who suffered a type IV tibial tubercle fracture with a type II Salter–Harris component who went on to develop compartment syndrome. This is a unique fracture variant from the Ogden classification. The fracture propagated from anterior to posterior through the secondary and then primary ossification center, while exiting the metaphyseal bone posteromedially; thus, representing a Salter–Harris type II variation to the type IV tibial tubercle fracture.
CASE DESCRIPTION
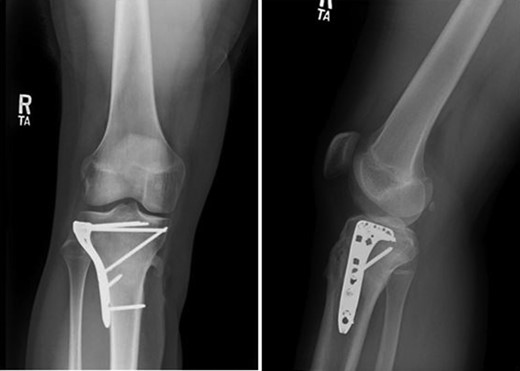
Patient is a 14-year-old male who slipped and fell while jumping off of a diving board and landed onto a flexed right knee. The patient was stable on presentation and neurovascularly intact with the knee locked in flexion. Skin was tenting anteriorly over the tibial tubercle and his compartments were swollen but compressible. A single plain film view (Fig. 1) was obtained prior to orthopaedic consultation. Closed reduction under sedation and splitting was attempted in the ED with partial but unsatisfactory improvement. Post-reduction radiographs (Fig. 2) demonstrated a tibial tubercle fracture with extension through the entire proximal tibial physis with metaphyseal involvement posteromedially. We classified this as a type IV tibial tubercle fracture, Salter–Harris II variant. In conjunction with patient and family we planned for urgent closed versus open reduction and application of knee-spanning external fixator. Immediately prior to surgery in the pre-operative holding area, the patient noted increasing right leg pain. In the operating room (OR), a marked increase in swelling with tense skin was observed. Due to rapidly progressive swelling and nature of the fracture, the decision was made to proceed with a 4-compartment fasciotomy of the right leg. The medial-sided fasciotomy (Fig. 3) revealed significant bulging of the superficial and deep compartments; however, the anterior and lateral compartments were less swollen. The fracture was unable to be closed reduced intraoperatively, therefore proximal extension of the medial fasciotomy wound was performed to open and reduce the fracture under direct visualization. Anatomic reduction was achieved and a knee-spanning external fixator was applied (Fig. 4). Approximately 72 hours later the patient was brought back to the OR for irrigation and debridement, lateral wound closure, and medial wound vacuum placement. Another 72 hours later, he returned to the OR for removal of the external fixator, ORIF, and split-thickness skin grafting of the medial fasciotomy site. An anterolateral approach was used with a 3.5 mm proximal tibial locking plate (Fig. 5). At most recent follow-up (Fig. 6), six months post-op, the patient is pain free, ambulating without assistive device, and has returned to all desired activities.

Presenting plain film view demonstrating proximal tibia fracture.

AP and lateral radiographs after attempted closed reduction which reveal type IV tibial tubercle fracture with posteromedial metaphyseal extension (Salter–Harris II variant).

Medial fasciotomy wound revealing bulging musculature with subsequent extension of the incision for reduction.

AP and lateral radiographs following open reduction and application of knee-spanning external fixator.

AP and lateral intraoperative fluoroscopic images following ORIF with proximal tibial locking plate.
DISCUSSION
The Ogden classification, a modification of the original Watson-Jones classification system, is the most accepted classification system for tibial tubercle fractures with five types described. Type IV fractures classically involve the entire proximal tibial physis. This fracture demonstrated some variation with regard to the Ogden classification by propagating into the metaphysis as it extended posteriorly. A pattern like this represents a unique Salter–Harris type II component to this type IV tibial tubercle fracture. This is somewhat predictable, due to the closure pattern of the physis in a posterior to anterior direction, and represents a transitional fracture similar to a triplane or tillaux fracture. Typical type III fractures further justify this logic as these represent transitional fractures that extend into the articular surface as opposed to the metaphyseal bone, again due to the posterior to anterior closure of the proximal tibial physis. Though seldom, this variation has been reported in the literature. Brey et al. [3] reviewed 53 patients with tibial tubercle fractures in a case series and reported a 28% prevalence of posterior metaphyseal involvement. They went on to report higher complication rates associated with these fracture patterns including compartment syndrome and refracture. However, they did not stratify by fracture classification.
Compartment syndrome is a potentially devastating sequelae that can often accompany acute tibial tubercle fractures – as seen in this case. Reported rates of compartment syndrome vary in the literature. Pretell-Mazzini et al. [6] reported a rate of 4%, while Frey et al. [7] reported a rate of 20%. Palokoff et al. [8] reported a 17% incidence of compartment syndrome. As previously discussed, Brey et al. [3] reported an increased rate of complications, including one case with compartment syndrome, in those with posterior metaphyseal involvement. The relatively high rate of associated compartment syndrome with tibial tubercle fractures can be attributed to the tributaries of the recurrent anterior tibial artery that course along the lateral border of the tubercle and can become trapped within the fascia and muscles of the anterior compartment after being avulsed [9]. The compartment release needs to be done urgently and priority should be given to realignment and releasing of the soft tissues including the vascular structures from the fracture site. If equipment and expertise, for definitive fixation of complex knee fractures, is not available at the time of reduction or if local conditions are not ideal, we recommend a two-stage approach with initial external fixation and optimization of soft tissues followed by delayed internal fixation.
Outcomes following appropriately managed tibial tubercle fractures have generally been excellent. Pretell-Mazzini et al. [6] conducted a systematic review of 325 patients with tibial tubercle fractures. They reported a 99.4% rate of radiographic union rate with 98% returning to preinjury activity levels with full range of motion. Pace et al. [2] reported 100% fracture healing with no growth disturbances in his series of 24 patients with type IV tibial tubercle fractures. In this case, subsequent radiographs have demonstrated fracture union without hardware complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No grants or financial support was received for this work.



