-
PDF
- Split View
-
Views
-
Cite
Cite
Igor Vaz, Lenny Starforth, Damiano Pizzol, Anna Claudia Colangelo, Vescicovaginal fistula management in low-income setting: a complicated case report, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz198, https://doi.org/10.1093/jscr/rjz198
Close - Share Icon Share
Abstract
Obstetric vescicovaginal (VVF) fistulas, most of all as consequences of prolonged neglected obstructed labor, occurs mainly in low-income countries. Considering the limited resources, both of trained specialists and equipments, fistulas have a devastating impact on affected women and their families from physical, social and economic point of view. However, also in low-income settings, fistulas prevalence and consequences could be reduced with focused interventions addressed to pregnant women during antenatal visits and to surgeons which face of these particular diseases. We report a case of obstetric VVF, related to a prolonged labor, treated by surgery and managed with satisfying results in a low-income setting.
INTRODUCTION
Genitourinary fistulas are abnormal communications extending between the urinary and the genital tract and can be acquired or congenital, with involuntary escape of urine into the vagina. There are many types of fistulas: vesicovaginal (VVF), vesicourethrovaginal, vesicouterine, vesicocervical, urethrovaginal, ureterovaginal, ureterouterine, and ureterocervical [1]. VVF is the most common type and, in low-income setting, it mainly results from neglected prolonged obstructed labor, which is associated with tissue ischemia, due to prolonged compression of the bladder and vagina by the fetus presenting part against the bony pelvis [2]. It affects more than 2 million women worldwide, with at least 50,000–100,000 new cases occurring annually [3].
The main symptom is the uncontrolled passage of urine through the vagina, purulent, foul-smelling vaginal discharge, dyspareunia, perineal pain, vaginal irritation and recurrent genitourinary tract infections. The most common management of VVF is to perform a ‘delayed’ surgical closure following a period of prolonged catheter drainage, a process, which allows necrotic and inflammatory material to slough and for local inflammatory responses to subside. Using this approach, a small proportion of fistula may close spontaneously as a result of catheter drainage alone, while those that do not heal can be treated surgically [4].
Obstetric fistulas have a devastating impact on affected women and their families from physical, social and economicpoint of view [5]. We report a case of obstetric VVF, related to a prolonged labor, treated by surgery and managed with satisfying results in a low-income setting.
CASE REPORT
A 26-year-old black woman was admitted to the Maputo Central Hospital with a VVF with anal sphincter rupture, perineal laceration and necrosis of inferior 1/3 of the bladder and cervix. Before arriving to medical attention, she underwent to 13 hours of obstructed labor resulting with an 11 months dead male fetus weighing 4600 g in a district hospital ended with cesarean section.
She underwent a necrectomy 1/3 inferior wall of the bladder and a lateral colostomy of the descending colon. After 4 weeks she was discharged with a stoma bag. After 2 weeks, she was admitted to Maputo Central Hospital to perform a complex reconstruction of bladder, vagina and anal sphincter. At the same time, we decided to close the colostomy. A hysterectomy of the remaining uterus after the necrectomy was done as the remaining uttering tissue was insufficient for uterine implantation. A sigmoid neobladder was created by removing a 30–35 cm sigmoid segment which was detubularized along the antimesenteric border. Then it was sutured to form a cylinder and after closure of the posterior and anterior walls the reservoir was rotated upside-down and 180° horizontally. A seromuscular window was cut and the mucosa was everted to create a neobladder neck. Then ureters are pulled through the sigmoid mesentery and anastomosis of ureter to the reservoir was performed creating a submucosal tunnel. Finally the upper wall of the reservoir was closed and anastomosis of the neobladder to the urethra was performed. Second step of the surgical procedure was the reconstruction of neovagina using descending colon with the closure of the posterior wall as there was no cervix or uterine connection. A segment of 10 cm long descending colon was transected preserving vascularization. The segment was rotated into the antiperistaltic position to reach the vaginal introitus. The proximal end of colon was pulled through the vaginal introitus and a prolapse of colon protruding more or less 3 cm out of the introitus was created and sutures were placed between the colonic wall and introitus. Third step of the procedure was an overlapping anal sphincteroplasty in order to reconstruct sphincter and perineal laceration. We mobilized the anoderm from the underlying sphincter mechanism and scar area. The sphincter was then isolated from its bed paying attention to preserve the branches of pudendal nerve. The sphincter mechanism was sectioned transversely through the middle of the scar and overlapped to snug up the anal aperture. Mattress sutures were carefully placed to maintain the desired opening size and the anoderm was carefully sutured over the sphincter with interrupted sutures. Finally the reconstruction of the colon continuity with a colon-rectal end to end manual anastomosis was performed In Fig. 1 are reported four steps of the complicated surgery. She was discharged after 21 days. On the fifth month, the patient developed an intermittent overflow incontinence with neo-bladder capacity of up to 1100 ml. Auto catheterization was opted for and is now being used by the woman to void her bladder from time to time with high fluid consumption to avoid bladder stones due to stasis. This has been so far the only complication.
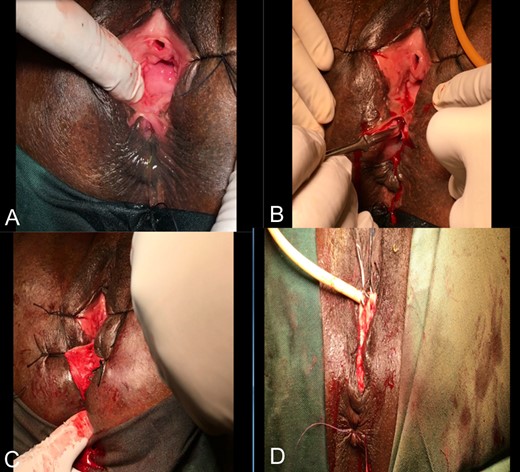
(A) VVF with perineal body (almost inexistent) laceration; (B) Perineal body excision; (C) Rectal exam on anal sphincter; (D) Closed VVF, restructured anal sphincter and perineal body.
DISCUSSION
The successful management of VVF depends most of all from the fistula characteristics and from early presentation and management. We presented a particular and extreme case of VVF as a result of the absence of antenatal visits and the consequent presentation of a pathological fetus, and the weakness of local health system that impeded an adequate and properly management. Nevertheless, during the intervention and the follow-up, no complication occurred, except a pressure incontinence of the new bladder. This represents the only limitation of the intervention, persisting to date after almost 2 years of follow-up. The patient voiding is therefore through auto-catheterization. The retention seems to be caused by either, a highly placed pubo-vaginal sling, a stenotic urethra or a neurogenic bladder. The patient during retention experiences pain in both flanks and auto-catheterization helps reduce the pain. This gives the clinical suspect of hydronephrosis diagnosis. To correct this phenomenon, the patient would have to be re-operated. With auto-catheterization, the patient feels in control and voids at her own convenience. The patient is psychologically traumatized against any more surgical interventions since the first surgery in the district hospital went wrong, losing her baby, urine and incontinent to feces. This case highlighted some crucial and dramatic health aspects: absence of adequate prenatal visits, weakness of health care network, long distances to health facilities, transportation and connection limitation alongside extremely poor road conditions, low health worker capacity, especially in rural context due to poor training and lack of motivation in fistula operations. Thus, on one side it is mandatory to fight many socio-cultural aspects as stigma, myths, superstitions and traditional healers that turn away patients from conventional medicine. On the other side, it is urgent to strengthen the health system in terms both of health care and prevention particularly, considering the high prevalence of obstetric fistulas should be necessary to develop ad hoc and high-quality services able to face of these diseases in order to render women a good quality of life. In conclusion, community reintegration of fistula patients is of paramount importance in a way of curbing devastating stigma and preventing recurrence of the same. Moreover, motivating and frequent retraining rural health staff should be taken into consideration in prevention of obstetric fistula in high prevalence locations incidences.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICS STATEMENT
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.



