-
PDF
- Split View
-
Views
-
Cite
Cite
Yohei Kawatani, Akari Tajima, Kotomi Takahashi, Shinya Watanabe, Atsushi Oguri, Subpectoral pacemaker implantation under tumescent local analgesia, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz193, https://doi.org/10.1093/jscr/rjz193
Close - Share Icon Share
Abstract
Tumescent local analgesia (TLA) is an anesthetic technique used for inducing local analgesia over large areas and is rarely used in cardiothoracic surgery. An 83-year-old, extremely thin woman was hospitalized with sick sinus syndrome, requiring pacemaker implantation. We chose a subpectoral mode of implantation to prevent skin complications. General anesthesia was deemed risky due to the history of chronic pulmonary disease; therefore, the operation was successfully performed under TLA. Moreover, TLA helped introduce a subpectoral pocket for implanting the pacemaker with minimal trauma and bleeding. The analgesia was sufficient, with minimal postoperative pain, and required no additional sedatives and analgesics. The patient was discharged without any complications.
INTRODUCTION
Pacemaker implantation requires local analgesia for the subcutaneous pocket method and general anesthesia for the subpectoral method. Tumescent local analgesia (TLA) is used for inducing local analgesia in large areas of the body using large volumes of diluted local anesthetic solution (xylocaine) combined with vasoconstrictors (epinephrine). TLA is used in various surgeries including plastic surgery and vascular surgery [1, 2]. However, only few studies have reported the use of TLA for cardiac implantable electronic device (CIED) implantation, including permanent pacemaker implantation. Here we report a case of subpectoral pacemaker implantation under TLA.
CASE PRESENTATION
An 83-year-old woman was brought to our emergency room with recurrent syncope, dyspnea, and lower extremity edema. She had a history of chronic obstructive pulmonary disease (COPD), and her symptoms began 2 months ago, when she developed bradycardia (heart rate: 30–70 bpm), and kept worsening.
We diagnosed syncope and heart failure caused by sick sinus syndrome and initiated temporary extracorporeal pacing, following which the syncope disappeared.
Permanent pacemaker implantation was indicated. Owing to her thin stature (body weight: 28 kg, height: 140 cm, body mass index: 14.3 kg/m2), subpectoral mode of pacemaker implantation was preferred over the subcutaneous pocket mode. Although general anesthesia is preferred for subpectoral pacemaker implantation, her history of COPD made its administration extremely risky. TLA, which provides sufficient analgesia over a broad area, was administered, and subpectoral implantation was performed.
Ultrasound-guided TLA administration was performed on the left upper precordium. TLA solution (430 mL normal saline, 20 mL sodium bicarbonate, 50 mL 1% xylocaine, and 0.5 mg epinephrine) was infused around the axillary vein and artery, subpectoral area, pectoralis major, and subcutaneous tissue along the planned-incision line (Fig. 1). A total of 75 mL TLA solution was infused under ultrasound and X-ray guidance below the pectoralis major, where the pocket for the pacemaker was to be created (Fig. 2).
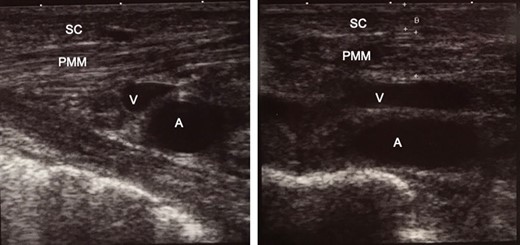
Intra-operative ultrasound examination for confirming the position of organs before infusion of tumescent local analgesia solution. The thickness of the subcutaneous tissue, 2.6 mm; and pectoralis major muscle, 5.6 mm. (a) The right side of the picture is the superior (head) side of the patient. (b) The right side of the picture is the right side of the patient. SC, subcutaneous tissue; PMM, pectoralis major muscle; V, axillary vein; A, axillary artery.
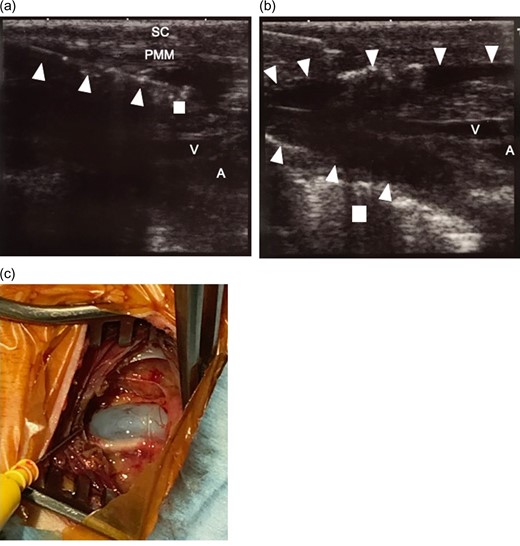
(a) Ultrasound-guided tumescent local analgesia technique. Tumescent local analgesic solution was infused under ultrasound image guidance. The 18-gauge needle can be easily identified (triangle. The tip of the needle is indicated by square.) and solution infusion can be observed. (b) After infusion of the solution. The area under the pectoralis major muscle was dissected and a pocket was made (surrounded by triangle) for placing the pacemaker. The surrounding tissue blood vessels were also dissected. Square indicates the first rib. c. Picture of the operation site after exposure of the axillary vein. Vasoconstriction of the axillary vein did not hinder the placement of the leads using purse string suture and Seldinger technique. The surrounding tissue is edematous because of tumescent local analgesia solution injection. But the we could easily identify the anatomical structures. The bleeding was limited due to the epinephrine in the tumescent local analgesia solution. SC, subcutaneous tissue; PMM, pectoralis major muscle; V, axillary vein; A, axillary artery.
An incision was made on the precordium, 4 cm long and 2 cm beneath the clavicle. The subcutaneous tissue was cut, and the pectoralis major was divided with electronic cautery. The pectoralis minor was partially cut for better exposure of the axillary vein.
Purse string sutures were introduced on the subclavian vein for placing the sheath and pacemaker leads. A subpectoral pocket was made by manually dissecting beneath the pectoralis major. This procedure was easy owing to TLA solution was dissected the subpectoral area. Additionally, the bleeding was limited due to the presence of epinephrine in the TLA solution, aiding hemostasis.
Pacemaker leads were inserted into the axillary vein using purse string suture and Seldinger technique, and placed at appropriate positions. The generator (Azure XT DR MR, Medtronic Inc., Minneapolis, MN, USA) was placed in the subpectoral pocket, and the wound was closed using buried suture. The operation was successfully performed with the exclusive use of TLA, with almost no blood loss. No additional analgesics and sedatives were needed intraoperatively. The patient did not complain of postoperative pain until 18 hours post-surgery, following which oral analgesics were administered. The patient was discharged 6 days after the surgery without any complications. No postoperative skin complication was noted.
DISCUSSION
Subcutaneous implantation of CIED is a risk factor for skin complications in the implantation pockets, especially, in thin patients [3, 4], whereas subpectoral implantation of devices presents a lower risk [5]. Our patient’s BMI was extremely low at 14, and her subcutaneous tissue was very thin at 2.6 mm; therefore, subpectoral implantation was preferred.
General anesthesia is widely used for subpectoral implantations; however, our patient had a higher risk of adverse effects for the use of general anesthesia because of COPD.
TLA employs the infusion of large volumes of diluted xylocaine, with epinephrine, in a broad area. It presents the advantage of providing sufficient analgesia in a broad area, whereas, the epinephrine helps hemostasis, and the analgesia persists for longer duration even after the operation [1, 6, 7]. Additionally, water-dissection, with reduced trauma and bleeding, can be performed with TLA [7]. These points improve the usefulness of TLA in subpectoral implantation of pacemakers, which involves incision of the pectoralis major and its fascia with resultant hemorrhaging in the pocket, which can be tedious. No additional sedatives and analgesics were needed following ultrasound-guided TLA, and no hemorrhaging was observed on dissecting the pocket during the operation. Additionally, the post-operative pain was minimal.
The epinephrine in TLA facilitates vasoconstriction [8]. The vasoconstriction in small vessels was sufficient to achieve hemostasis, however, constriction of the axillary vein did not complicate the introduction of the leads (Fig. 2).
In conclusion, TLA was extremely useful for subpectoral pacemaker implantation in a thin patient. Further investigations are needed to investigate its effectiveness of inducing anesthesia in healthy patients.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Self funded.
ETHICAL APPROVAL STATEMENT
This study was approved by local ethical committee (approval number THH01-01).
DECLARATION OF INTEREST
No conflict of interest.



