-
PDF
- Split View
-
Views
-
Cite
Cite
Danny Issa, Yahya Alwatari, George B Smallfield, Rachit D Shah, Spontaneous transmural perforation in eosinophilic esophagitis: RARE case presentation and role of esophageal stenting, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz190, https://doi.org/10.1093/jscr/rjz190
Close - Share Icon Share
Abstract
Eosinophilic esophagitis (EoE) is a rare disease of the esophagus that is characterized by eosinophilic infiltrate within the esophageal mucosa resulting in chronic inflammation and stenosis. It typically presents with symptoms of esophageal dysfunction with dysphagia and food impaction being the most common presenting complaints. Herein we describe a rare case presentation of a young patient with spontaneous esophageal perforation in the setting of undiagnosed EoE. We suggest that the placement of a covered esophageal stent can provide full closure of the perforation and restoration of the integrity of the GI tract without the need for more invasive open repair. The patient had a short recovery time with no reported postoperative complications upon 30 months follow up. We believe that it’s important to consider and rule out EoE in patients with a history of dysphagia and esophageal perforation.
INTRODUCTION
Eosinophilic esophagitis (EoE) is a clinicopathologic disease of the esophagus that is characterized by eosinophilic infiltrate resulting in chronic inflammation. It was first reported as an allergic disease in 1995. Although originally considered a rare condition, the incidence has increased over the last two decades, with an estimated pooled prevalence of 56.7 per 100,000 people in the United States [1].
Pathologically the presence of eosinophil-predominant inflammation with 15 eosinophils/high power field is considered a minimum threshold for the diagnosis of EoE. Clinically, EoE is characterized by symptoms related to esophageal dysfunction. In addition to dysphagia, heartburn, and chest or abdominal pain, solid food impaction is one of the most common presentations of EoE. In fact, studies have suggested that a significant number of patients presenting for the first time with food impaction have underlying pathologic features consistent with EoE [2].
Spontaneous esophageal perforation as a primary manifestation of EoE is very rare. A few cases have been reported in the literature with variation in the primary treatment method [3, 4]. The presence of esophageal stenosis, prolonged symptoms and higher density of eosinophilic infiltration are potential risk factors for rupture in EoE [4, 5].
CASE REPORT
A 32-year-old Caucasian male presented with sudden onset of a chest and epigastric pain. His past medical history was significant only for a personal and family history of polycystic kidney disease. Upon arrival at the emergency department, the patient was hypoxic and tachycardic. Physical examination was significant for bilateral subcutaneous emphysema present over the lateral aspects of the neck. His abdomen was soft and not distended.
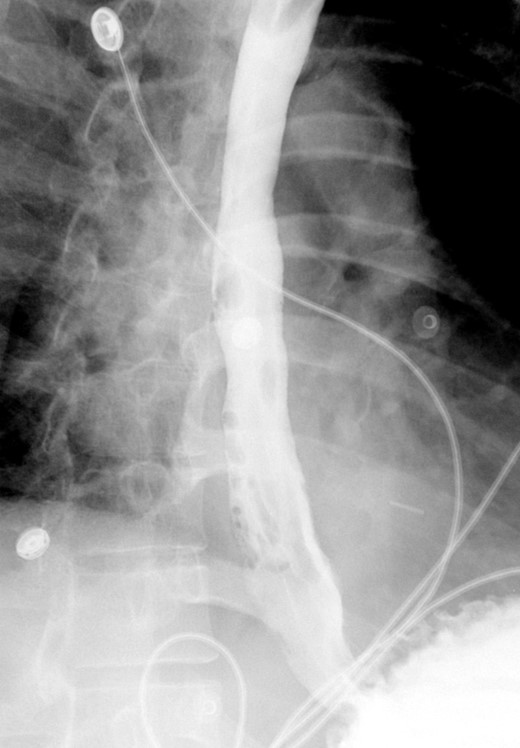
A computed tomographic scan revealed air and fluid surrounding the esophagus (Fig. 1). Esophagogram performed with water-soluble contrast media showed a distal esophageal perforation with a free leak into a large mediastinal cavity to the left of the esophagus (Fig. 2). The patient was triaged directly to the operation room. A left chest tube was placed with improvement in his oxygenation, and grossly murky fluid was drained. Esophagogastroduodenoscopy (EGD) was performed next and revealed a very small caliber esophagus with concentric ringed appearance. A tight stricture was noted in the mid-esophagus, which only allowed passage of a pediatric gastroscope. In the lower esophagus, a 2-cm tear with necrotic edges was visualized 3 cm above the gastroesophageal (GE) junction. With this diffusely strictured and very diseased appearance of the esophagus, the decision was made to proceed with stent placement and thoracoscopic drainage of the mediastinum rather than primary surgical repair via thoracotomy. A fully covered, 15 cm × 19 mm, EndoMAXX® esophageal stent was successfully placed covering the perforation site. Mediastinal washout and drainage was performed subsequently via left thoracoscopy. A postoperative esophagram showed no leak and the patient was started on a liquid diet that was tolerated well. His hospital stay was uneventful, and he was discharged on twice daily high-dose proton pump inhibitor (PPI) on post-operative Day 5. He was placed on a mechanical soft diet on discharge. Repeat upper GI study with water soluble contrast postoperatively showed no evidence extravasation. (Fig. 3)
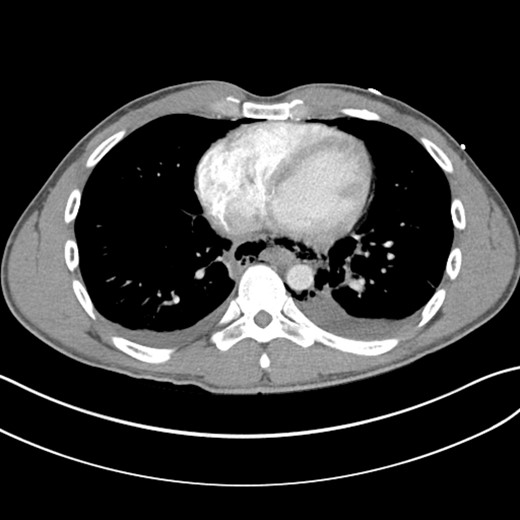
Shows evidence of esophageal rupture and leak with pneumomediastinum and air and fluid surrounding the esophagus.

Demonstrates narrow esophageal caliber and extensive distal left thoracic esophageal leak approximately 3 cm proximal to the GE junction.

Shows metallic expandable stent in a satisfactory position in the mid to lower thoracic esophagus extending to the GE junction. Water-soluble contrast is seen filling the stent with no evidence of extravasation.
A follow-up EGD was performed 6-weeks later for stent removal. Although the stent had migrated slightly, it continued to cover the previous perforation site. The stent was removed, and the esophagus appeared well healed with no residual tear. Contrast study showed no residual leak or significant stricture (Fig. 4). On follow-up endoscopy, biopsies from the proximal and distal esophagus revealed 20 eos/hpf and 30 eos/hpf, respectively. The patient was kept on PPI and started on topical steroids and continued to do well with no reported symptoms on the last follow up 9 months and two years and a half after the initial presentation.
Shows interval removal of the esophageal stent with no evidence of an esophageal leak.
DISCUSSION
The increased understanding of the pathogenesis of EoE and the range of potential complications of this esophageal disorder have led to substantial advances in both medical and surgical management. A large body of literature is currently available to support the efficacy of steroids and food elimination diet for the medical therapy of EoE. Histologic response rates have been reported in the 50–90% range for topical steroids and around 75%for the six-food elimination diet [6]. Targeted biologic therapy such as anti-IL-5 and anti-IL-13 have been studied in randomized trials and shown benefit in steroids-refractory patients [7]. Endoscopic intervention is frequently required to manage food impaction; a common presenting symptom of EoE.
One of the feared complications of EoE is esophageal perforation. Only a few cases of spontaneous rupture of the esophagus, also known as Boerhaave syndrome, have been reported in patients with EoE [4, 5]. The presence of eosinophilic infiltrate is the likely mechanism responsible for the progression of epithelial inflammation to fibrostenotic disease causing esophageal remodeling [8]. This remodeling can lead to impaired motility and results in frequent episodes dysphagia and food impaction and as damage progress spontaneous perforation can happen.
The goals of perforation treatment are to control the esophageal leak, drain the contaminated mediastinum, provide adequate enteral nutrition and eventually restore the continuity of the GI tract. Two interventional approaches can be used; endoscopic stenting vs traditional open repair, either via thoracotomy or laparotomy based on the location of esophageal tear. Esophageal stent placement was compared to surgical repair in a study of 60 propensity-matched patients with iatrogenic esophageal perforation. Stent placement was found to be associated with a shorter ICU stay and shorter overall hospital length of stay. Cost and time to resumption of oral intake were also significantly better in the stent group [9]. Runge et al. recently published a 14 years retrospective cohort study on the causes and outcome of esophageal perforation in EoE [5]. They reported 2% (n 10) rate of perforation with most occurring after a prolonged food impaction. Four of these patients were managed operatively and six underwent conservative management. None of the patients were managed with minimally invasive surgical approaches or endoscopic stenting.
CONCLUSION
▪ Consider underlying EoE in patient with spontaneous esophageal perforation.
▪ Minimally invasive treatment through the placement of a covered esophageal stent and drainage of the mediastinum should be considered.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- stents
- boerhaave's syndrome
- deglutition disorders
- postoperative complications
- esophageal diseases
- constriction, pathologic
- esophageal perforation
- follow-up
- esophagus
- gastrointestinal tract
- eosinophilic esophagitis
- esophageal mucous membrane
- chronic inflammation
- esophageal stents
- esophageal food impaction
- infiltrates
- transmural
- rare diseases
- undiagnosed
- personal integrity



