-
PDF
- Split View
-
Views
-
Cite
Cite
Simmi Patel, Armand Asarian, Philip Xiao, Clear cell papillary renal cell carcinoma: a case report and literature review, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz177, https://doi.org/10.1093/jscr/rjz177
Close - Share Icon Share
Abstract
Clear cell papillary renal cell carcinoma (CCPRCC), a type of low-grade renal cell neoplasm was recently included in the 2016 WHO classification of renal tumors (Tickoo SK, dePeralta-Venturina Mariza N, Harik LR, Worcester Heath D, Salama ME, Young AN et al. Spectrum of epithelial neoplasms in end-stage renal disease: an experience from 66 tumor bearing kidneys with emphasis on histologic patterns distinct from those in sporadic adult renal neoplasia. Am J Surg Pathol 30:141–153, 2006). While being recognized as its own entity, there is little research on CCPRCC. The specific tumor comprises of 9.3% of all renal tumors in young adults with an age range of 18-88 years (Wang Y, Ding Y, Wang J, Gu M, Wang Z, Qin C et al. Clinical features and survival of clear cell papillary renal cell carcinoma: 10-year retrospective study from two institutions. Oncology letters 16:1010–22, 2018.). In this article we provide recent understanding of CCPRCC and how to identify its distinct pathological entity. It is strongly positive for cytokeratin 7 (CK7), vimentin and mostly negative for CD10 and AMACR (Zhanyong B and John TE Clear cell papillary renal cell carcinoma in bilateral native kidneys after 2 year of renal transplantation: report of a case and review of literature. Case Reports in Transplantation 2011:11–4, 2011). Histopathologically, all cases of CCPRCC exhibited a tubular and papillary architecture, cuboidal tumor cells with clear cytoplasm and low Fuhrman grade (Wang Y, Ding Y, Wang J, Gu M, Wang Z, Qin C et al. Clinical features and survival of clear cell papillary renal cell carcinoma: 10-year retrospective study from two institutions. Oncology letters 16:1010–22, 2018; Kuroda N, Ohe C, Kawakami F, Mikami S, Furuya M, Matsuura K et al. Clear cell papillary renal cell carcinoma: a review. Int J Clin Exp Pathol 7: 7312–18, 2004.; Srigley JR, Delahunt B, Eble JN, Egevad L, Epstein JI, Grignon D, et al. The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. Am J surg Pathol. 37:1469–89, 2013). This case report and literature review highlights the cryptomorphic, immunohistochemical and cytogenic features of CCPRCC which will assist in understanding and managing these tumors.
INTRODUCTION
Clear cell papillary renal cell carcinoma (CCPRCC) was recently established as one of the five new distinct and unique renal entities by the Classification Working Group of the International Society of Urological Pathology in a conference held at Vancouver, Canada [5]. In 2006, Tickoo et al. described CCPRCC as a subtype of renal tumor of patients with end stage renal disease (ESRD) [1]. However, currently CCPRCC has also been shown to occur in healthy and functional kidneys as well [7].
Despite CCPRCC being a common type of RCC, there is little understanding of the nature of the tumor. CCPRCC is a low-grade RCC which is strongly positive for cytokeratin 7 (CK7) and mostly negative for CD10. Genetically CCPRCC is associated with no deletion of 3p (Von Hippel Lindau gene- VHL) or loss of chromosome 5. Additionally, there are no gains of chromosome 7, 17 or chromosomal abnormalities [6]. Morphologically, this tumor can be solid or cystic depending on the architectural arrangements. The neoplastic cells have clear cytoplasm with low nuclear grade [4]. Features include the presence of papillary or tubular structures lined by single layer of clear cells with nuclei arranged from the basement membrane [7].
Clinically, the number of cases and follow up reports concerning CCPRCC seem small; however, the future is promising for more research in order to better understand this complex yet vastly interesting subtype of RCC. Therefore, the purpose of this study is to (1) analyze a case report of CCPRCC, (2) evaluate histological morphology and immunohistochemistry for CCPRCC and compare it to clear cell RCC and papillary RCC and (3) comment on future perspectives concerning the pathobiological aspects of CCPRCC.
CASE REPORT
This a case of a 79-year-old female with a past medical history of Hypertension, Diabetes Mellitus type 2, Hyperthyroidism s/p thyroidectomy, history of colon cancer s/p surgery as well as a previous incident of CCPRCC 10 years s/p right nephrectomy. Patient was admitted for left partial nephrectomy in 2018 for a suspected renal mass on the left kidney.
Pathological diagnosis confirmed CCPRCC. Grossly, the partial nephrectomy specimen measured 4 × 3.1 × 2.2 cm. The attached fatty tissue surrounding the kidney measured 10.5 × 7.8 × 2.5 cm. Cut sections showed a tan pink nodule with foci of white tan tissue measuring 3.5 cm. Microscopic examination reveals that the tumor is composed of cystic, tubular, solid and papillary components with clear cells and a low nuclear grade (Fig. 1). Tumor cells were also positive for CK7 (Fig. 2) and negative for CD10 (Fig. 3) and p504s supporting the diagnosis of CCPRCC.
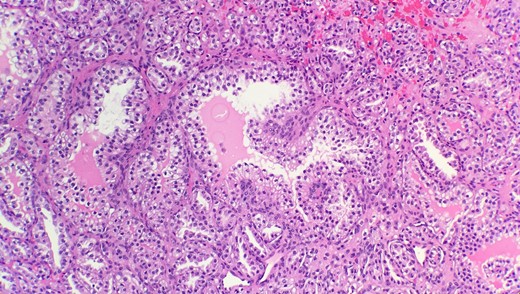
Microscopic examination reveals that tumor is composed of mixture of cystic, solid and papillary components clear cells with low nuclear grade (HE stain 20x).
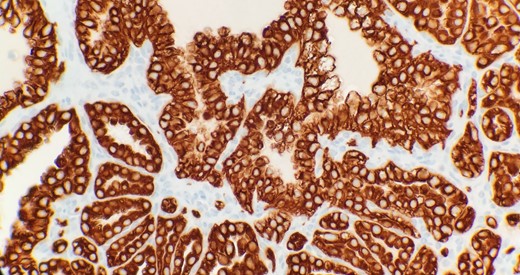
Immunohistochemical stain reveals that tumor cells are positive for CK7 (IHC 40x).
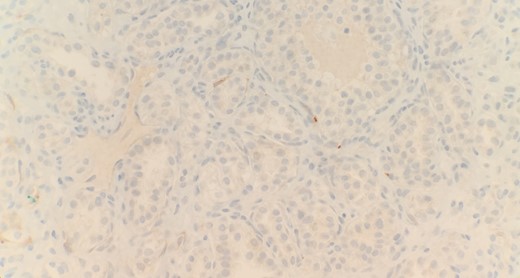
Immunohistochemical stain reveals that tumor cells are negative for CD10 (IHC 40x).
DISCUSSION
CCPRCC is a relatively newly recognized subtype of RCC. CCPRCC shares morphological features with several variants of RCC such as clear cell papillary and cystic RCC, renal angiomyoadenomatous tumor and sporadic RCC [8]. The morphological features of CCPRCC are vastly integrative. These tumors can be cystic with multiple growth patterns including cysts, tubules, acini, papillae and clear cell nests or could be non-cystic. The tubules, acini, ribbons or papillae are usually lined with a single layer of tumor cells. These tumor cells have clear cytoplasm with a low nuclear grade. The nuclei tend to be oriented away from the basement membrane facing the apical surfaces [1]. According to the Fuhrman criteria, nuclear atypia corresponds to grade 1 or 2. The fibrous stroma often demonstrates smooth muscle metaplasia [10].
The immunophenotype for CCPRCC is quite unique as well. These tumors often are diffusely positive for CK7 and negative for CD10 and AMACR (alpha-methyacyl-CoA racemase) [9].
In terms of genes, CCPRCC lacks genetic similarities to either clear cell RCC (CCRCC) or papillary RCC (PRCC). CCRCC is associated with the loss of chromosome 3p where the gene, Von Hippel-Lindau (VHL) and polybromo-1 (PBRM1) are translocated. On the contrary, PRCC is associated with trisomy of chromosome 7, 17 and loss of Y chromosome [2]. The tumor lacks a chromosome 3p deletion or polysomy of chromosomes 7 and 17 [3]. However, CCPRCC does not share any of these features. No mutation or methylation of VHL gene has been reported in cases of CCPRCC [10]. Aydin et al. report low copy number gains at chromosome 7 and 17 [6] while Kuroda et al. report polysomy for chromosome 7 and monosomy for chromosomes 17, 16 and 20 [10].
Due to the unusual nature of CCPRCC, it is important to differentiate clear cell RCC and papillary RCC from CCPRCC. Table 1 demonstrates the key features to differentiate between these rather unique tumors.
| . | Clear cell RCC . | Papillary RCC . | CCPRCC . |
|---|---|---|---|
| Microscopic | Architecturally and Cytologically diverse: solid, alveolar, acinar, cystic growth patterns of cells with clear or eosinophilic cytoplasm |
| Architecture shows wide range of structures: papillary tubules and solid acinar nests or ribbons. Papillary structures are lined by cells with clear cytoplasm. Nuclei are polarized away from basement membrane. |
| Immunohistochemical | |||
|
|
|
|
| Molecular | Chromosome 3p deletion VHL gene mutation | Polysomy of chromosomes 7 and 17 | Lack 3p deletion, VHL gene mutation and polysomy of chromosome 7 and 17 |
| . | Clear cell RCC . | Papillary RCC . | CCPRCC . |
|---|---|---|---|
| Microscopic | Architecturally and Cytologically diverse: solid, alveolar, acinar, cystic growth patterns of cells with clear or eosinophilic cytoplasm |
| Architecture shows wide range of structures: papillary tubules and solid acinar nests or ribbons. Papillary structures are lined by cells with clear cytoplasm. Nuclei are polarized away from basement membrane. |
| Immunohistochemical | |||
|
|
|
|
| Molecular | Chromosome 3p deletion VHL gene mutation | Polysomy of chromosomes 7 and 17 | Lack 3p deletion, VHL gene mutation and polysomy of chromosome 7 and 17 |
| . | Clear cell RCC . | Papillary RCC . | CCPRCC . |
|---|---|---|---|
| Microscopic | Architecturally and Cytologically diverse: solid, alveolar, acinar, cystic growth patterns of cells with clear or eosinophilic cytoplasm |
| Architecture shows wide range of structures: papillary tubules and solid acinar nests or ribbons. Papillary structures are lined by cells with clear cytoplasm. Nuclei are polarized away from basement membrane. |
| Immunohistochemical | |||
|
|
|
|
| Molecular | Chromosome 3p deletion VHL gene mutation | Polysomy of chromosomes 7 and 17 | Lack 3p deletion, VHL gene mutation and polysomy of chromosome 7 and 17 |
| . | Clear cell RCC . | Papillary RCC . | CCPRCC . |
|---|---|---|---|
| Microscopic | Architecturally and Cytologically diverse: solid, alveolar, acinar, cystic growth patterns of cells with clear or eosinophilic cytoplasm |
| Architecture shows wide range of structures: papillary tubules and solid acinar nests or ribbons. Papillary structures are lined by cells with clear cytoplasm. Nuclei are polarized away from basement membrane. |
| Immunohistochemical | |||
|
|
|
|
| Molecular | Chromosome 3p deletion VHL gene mutation | Polysomy of chromosomes 7 and 17 | Lack 3p deletion, VHL gene mutation and polysomy of chromosome 7 and 17 |
In summary, clear cell papillary renal cell carcinoma (CCPRCC) is a rather unusual and unique variant of renal cell carcinoma (RCC) which differentiates through its cellular architecture as well as molecular genetics. CCPRCC typically is CK7 positive and CD10 negative differentiating it from clear cell RCC and papillary RCC. CCPRCC also presents with low grade suggesting low metastatic potential. Due to the unconventional nature of the tumor, we suggest more research comparing multiple cases of CCPRCC to create a standard treatment plan for patients as well as to better understand the nature of such an integrative tumor.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- renal transplantation
- kidney failure, chronic
- adult
- cytoplasm
- kidney neoplasms
- medical oncology
- neprilysin
- surgical pathology
- signs and symptoms
- vimentin
- world health organization
- kidney
- neoplasms
- pathology
- transplantation
- tumor cells
- neoplasms, epithelial
- young adult
- papillary renal cell carcinoma
- keratin 7



