-
PDF
- Split View
-
Views
-
Cite
Cite
Sardar Hassan Arif, Ayad Ahmad Mohammed, Migrated intrauterine device presented as anterior abdominal wall abscess, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz174, https://doi.org/10.1093/jscr/rjz174
Close - Share Icon Share
Abstract
The migrated intrauterine contraceptive device can cause various presentations depending on the location, some may have late presentations like our case presenting after 5 years and after pregnancy and delivery by cesarean section. A 34-year-old lady had painful suprapubic mass for 1-week, with fever. She had history of intrauterine device (IUD) placed before 5 years. The patient became pregnant 1 year before presentation and delivery done by cesarean section. Examination showed a tender mass 3 cm above the scar of the previous cesarean section. The clinical picture was consistent with abdominal wall abscess. During surgery pus drained and the IUD extracted from the cavity of the abscess. High index of suspicion is needed when there is history of missed IUD and any abdominal complain. Abdominal X-ray and ultrasound will give better diagnostic value. Most cases need surgical extraction of the device which can be done laparoscopically.
INTRODUCTION
Intrauterine device is effective, reversible, and relatively safe method of contraception. It works by inducing a sterile inflammatory reaction in the uterine lining preventing implantation of the embryo. Hormone releasing devices causes atrophy of the uterine lining, impairs the motility of the cilia in the fallopian tubes, and make the cervical mucosa impermeable for the sperms. These effects may be primary or secondary however the modern devices act through hormonal and biological effects live inhibiting ovulation or by reducing the chance of the sperm to fertilize the ovum [1–3].
Complications of the IUDs include uterine bleeding, increased risk of ectopic gestation, pelvic inflammatory disease, uterine perforation, misplacement and migration of the device [1].
Displacement of the intrauterine device have been estimated to occur in around 5% of patients [4].
The clinical presentation of migration of the device depends on the location of the device. Cases have been reported that the IUD extracted from unusual locations like the broad ligament, abdominal wall, the inguinal region, the sigmoid colon, the urinary bladder, and the vermiform appendix [5–8].
X-ray is commonly used to localize the locating of the device, but the exact localization is sometimes very difficult, ultrasound can give more information about the site of the device in some cases, the combination of the two yields better diagnostic value. Hysteroscopy is used in some cases [1, 4, 9, 10].
CASE PRESENTATION
A 34-year-old lady presented to the surgical consultation department complaining from painful suprapubic abdominal mass for 1-week duration, the patient had fever mainly at night with anorexia. The patient has negative medical history. In the gynecological history taking she had history of intrauterine device placed 5 years before presentation. The patients planed for pregnancy but the threads of the device were missing. Hysteroscopy done and it showed an empty uterine cavity. The patient became pregnant 1 year before presentation and she delivered her baby by cesarean section.
Abdominal examination: there was a tender red and hot mass related to the abdominal wall and 3 cm above the scar of the previous surgery, the mass was constant in size during coughing and was not reducible. The clinical picture was consistent with abdominal wall abscess.
Surgery done under general anesthesia opening of the lump done which was containing thin pus and the cavity was found to contain the missed IUD (Fig. 1).
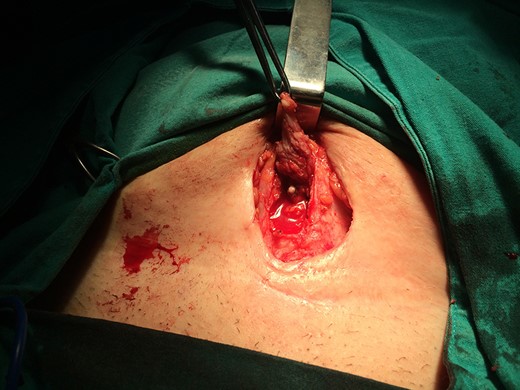
Intraoperative picture showing the cavity of the abscess opened containing thin pus with the IUD inside the cavity.
The device was trapped in the rectus sheath. Extraction of the IUD done and the cavity curated and washed with normal saline (Fig. 2).
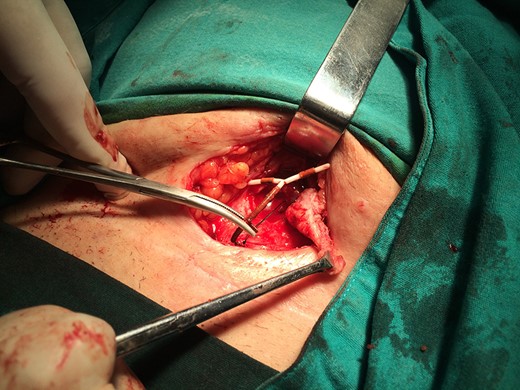
Intraoperative picture showing the IUD extracted from the abscess cavity.
The fascia closed with delayed absorbable suture material with partial closure of the skin done and a corrugated drain placed for 3 days. Oral antibiotics continued for 7 days and the patient had complete healing after 2 weeks.
DISCUSSION
Migration of the IUD is not clearly understood but may be due to perforation at the time of insertion or the expulsion of the device secondary to uterine contractions. It may also be caused by the local inflammatory reaction caused by the device especially copper containing devices [8].
The IUD can be extracted during pregnancy using the hysteroscopy without affecting the gestational sac by extracting the threads of the device [11].
Ultrasound is useful in detecting the complications associated with the use of IUD specially in complaining women [12, 13].
Some similar cases which presented with abdominal wall abscess have been reported and were treated with laparotomy and extraction of the device, in some cases it may associated with abdominal wall actinomycosis which is treated with extraction and antibiotics. When the IUD is misplaced inside the abdominal cavity, most cases are successfully extracted laparoscopically [7, 14, 15].
High index of suspicion is needed when there is history of missed IUD and any abdominal complain. Abdominal X-ray and ultrasound will give better diagnostic value. Most cases need surgical extraction of the device which can be done laparoscopically.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest to be declared.
FUNDING
The authors are the source of the funding.



