-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel R Principe, Andreea Raicu, Tova M Bergsten, Jonathan Rubin, Colleen Hagen, Ileal carcinoid tumor represents after prolonged remission as a solitary breast mass, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz171, https://doi.org/10.1093/jscr/rjz171
Close - Share Icon Share
Abstract
While the metastatic spread of breast cancer is well documented, the breast is seldom a site for metastasis. Non-mammillary cancers can involve the breast or axilla, though this is exceedingly rare with few reported instances. Here, we present the case of a 62-year-old woman who attended an outpatient breast clinic with a history of an ileal carcinoid tumor complicated by multi-organ metastasis. Her disease was in clinical remission for several years, though she recently re-presented with a single solitary lesion to the breast that was later confirmed as a recurrence of her carcinoid tumor. This serves as an important reminder that the breast can indeed be a site for metastasis. As metastatic breast lesions can often be difficult to diagnose, it is essential to obtain a thorough medical history in order to determine the appropriate clinical course.
INTRODUCTION
Non-mammary metastases to the breast are exceedingly rare. Though uncommon, such tumors are important to identify as the clinical management can differ significantly from primary breast cancers [1]. Secondary breast malignancies can be difficult to diagnose, particularly as most cases present as a solitary mass with a lack of pathognomonic features. Additionally, prognosis is generally poorer than primary breast cancers, and most patients with metastatic breast lesions often have additional metastases found on subsequent imaging [1]. Here, we describe the case of a patient with a prior history of an aggressive illeal carcinoid tumor complicated by metastases to liver and right breast. She was thought to be in complete remission, but re-presented several years later with a new left breast mass later confirmed as metastasis from the initial carcinoid tumor.
CASE REPORT
A 62-year-old woman was referred to an outpatient breast clinic after routine mammography identified a mass in her left breast. Her oncologic history was extensive, including an ileal carcinoid tumor in 2001. This was resected with negative margins, however, the patient re-presented with metastasis to her right breast in 2005. Her breast mass was treated with lumpectomy and radiation, though the patient would once again re-present with a metastatic carcinoid tumor involving the liver in 2011. This was managed with both Transarterial Chemoembolization (TACE) and Cryoablation. The patient responded well and subsequent scans were stable.
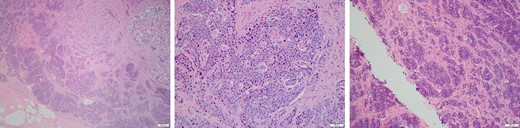
At this most recent visit, physical exam was unremarkable. The patient denied new symptoms including palpable masses, pain, nipple discharge/retraction, skin change, or lymphadenopathy. Diagnostic mammogram was concerning for a suspicious left breast mass (0.6 × 0.5 × 0.5 cm) at the 6:30 position located 4 cm from the nipple and categorized as BI-RADS 4 (Fig. 1). The mass was biopsied, and tissues sent to pathology for diagnosis. The morphology was consistent with the patient’s previous carcinoid tumor (Fig. 2), and tissues stained positive for CD56, CDX2, Chromogranin, and Synaptophysin (Fig. 3). Additionally, tissues were negative for CD117, Estrogen/Progesterone receptors (ER/PR), GCDFP, HER2-Neu, p63, and TTF-1. The tumor had a low proliferative index, with >2 mitoses per high power field. These findings supported a diagnosis of a metastatic, well-differentiated, Grade 2/3 neuroendocrine tumor.
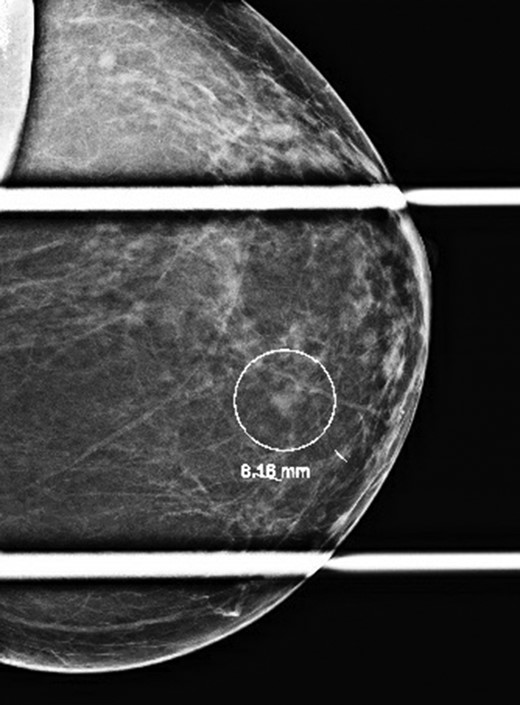
Diagnostic mammogram revealing a BI-RADS 4 left breast mass at the 6:30 position 4 cm from the nipple.
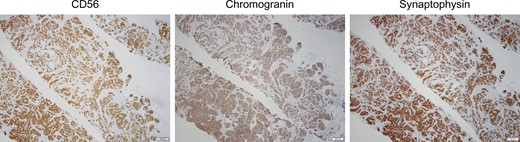
Tissues were stained for CD56, Chromogranin, and Synaptophysin expression, affirming a diagnosis of a metastatic ileal carcinoid tumor.
Given her history of an ileal carcinoid tumor, we next ordered an Octreotide scan, which showed no focal abnormality in the abdomen (Fig. 4). After discussing potential treatment options, following preoperative evaluation the patient underwent a left breast lumpectomy with wire localization. She tolerated the procedure well and is currently being managed through active surveillance.
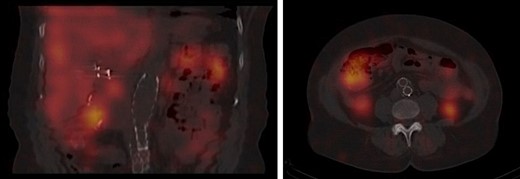
Octreotide scan showing normal accumulation in the liver, spleen, kidneys and bladder with no focal abnormality in the abdomen.
DISCUSSION
Breast cancer is the most common malignancy worldwide, with 2 088,849 new cases in 2018 [2]. As such, screening mammograms are an important part of female wellness. When a suspicious mass is identified on screening mammography as in our patient, the differential diagnosis is extensive, including a variety of benign and malignant conditions. These are almost ubiquitously primary breast issues, such as fibroadenomas, cysts, or breast cancers. However, in rare instances, breast masses can stem from extra-mammillary malignancies. These are generally associated with a poor prognosis compared to primary breast cancers, though outcomes vary considerably based on the etiology of the metastatic tumor.
Breast metastases have been observed in several extra-mammary malignancies including T and B cell lymphomas, cervical, colon, gastric, lung, nasal, ovarian, and thyroid carcinomas, melanoma, as well as a variety of carcinoid tumors [1, 3, 4]. As treatment varies so significantly for these conditions, it is imperative to diagnose breast metastases quickly in order to ensure the appropriate therapy is provided. To this end, there are several clinical and radiographic findings that can also be helpful in differentiating primary and secondary breast malignancies.
For instance, cancers that gain access to the breast via hematogenous spread typically present as a solitary circumscribed mass on mammography, whereas cancers that follow lymphatic dissemination may have associated edema or skin changes. Additionally, metastatic lesions to the breast are generally non-spiculated and lack skin or nipple retraction [5], as observed in many primary breast cancers [6]. However, in all cases, mammography is not sufficient for diagnosis. While additional imaging such as ultrasound, CT, or breast MRI are often helpful in risk stratifying patients, most concerning breast masses should be either biopsied or excised. When locally advanced or extra-axillary disease is suspected, additional whole body imaging such as a PET/CT may also be indicated [7].
As mentioned, extra-mammillary breast metastases can often lack clear defining features on histology, further complicating diagnosis. It is therefore imperative to obtain a thorough and comprehensive medical history, as this is often the most helpful factor when properly diagnosing a metastatic lesion to the breast. For instance, our patient had a history significant for an ileal carcinoid tumor complicated by multiorgan metastasis with several recurrences, one of which involved the right breast. Therefore, when a new left breast mass was identified on screening mammography, though the possibility of a new primary cancer was considered, a metastatic lesion was immediately suspect.
Carcinoid tumors comprise a group of related neuroendocrine cancers, most frequently affecting the gastrointestinal (GI) tract. As carcinoid tumors are often slow growing, many are diagnosed incidentally, though larger tumors may cause chronic abdominal pain, bowel obstruction, or early satiety. In rare instances, patients may complain of flushing and diarrhea. These symptoms comprise a paraneoplastic ‘Carcinoid Syndrome’, and are most often associated with metastatic tumors originating in the distal small intestine or proximal colon [8].
Classically, these carcinoid tumors will metastasize to other parts of the GI tract. However, GI carcinoid tumors occasionally involve distant organs including the breast [9, 10]. Most frequently, these solitary breast lesions are the first clinical signs of an underlying carcinoid tumor, and are found on routine physical exam. Bilateral breast metastases as seen in our patient are even less common, with very few reported cases. As such, when suspicious breast masses are identified and lack histologic features of primary breast disease, a metastatic carcinoid tumor should be included on a differential diagnosis, particularly in a patient with a prior history of metastatic disease.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
D.R. Principe is supported by the National Cancer Institute of the National Institutes of Health under Award Number F30CA236031.
CONFLICT OF INTEREST DISCLOSURE
The authors have no conflicts to disclose.



