-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroyuki Yamada, Yasunori Takeda, Yu Ohashi, Ryousuke Abe, Ikuya Miyamoto, Oral diverticulum: a case report with histopathological findings, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz170, https://doi.org/10.1093/jscr/rjz170
Close - Share Icon Share
Abstract
Oral diverticulum is rarely encountered, and the histopathological findings are unclear. We herein report a case of an oral diverticulum and describe its histopathological findings. A buccal mucosal outpouching was observed in a 66-year-old man. Food debris was seen within the outpouching. Under the clinical diagnosis of a diverticulum-like lesion, excision of the outpouching was performed through an intraoral incision to stop food impaction. Histopathological examination revealed that the excised lesion was a true diverticular structure composed of a keratinising, squamous epithelial lining with a surrounding fibrous connective tissue wall, with inflammatory cell infiltration and haemorrhage. The histopathological diagnosis was a diverticular pouch of the buccal region. Clinicians should be aware of this lesion to ensure correct diagnosis and treatment.
INTRODUCTION
A true diverticulum is a blind outpouching of the alimentary tract that communicates with the lumen and includes all three layers of the bowel wall. The most common congenital diverticulum is Meckel’s diverticulum of the ileum [1]. Conversely, the most common acquired diverticula are located in the sigmoid colon [1]. These congenital or acquired diverticula are uncommon lesions that are usually asymptomatic but sometimes lead to recurrent infection, massive bleeding, or perforation to the abdominal cavity [1, 2]. A diverticulum is rarely encountered in the oral cavity, and clinicians are unfamiliar with this lesion. Therefore, clinical diagnosis is not easy for dental practitioners. To date, only six cases have been reported in the English-language literature [3–8]. Moreover, the histopathological findings of this lesion are not fully understood. We herein report a case of oral diverticulum and describe its histopathological findings.
CASE REPORT
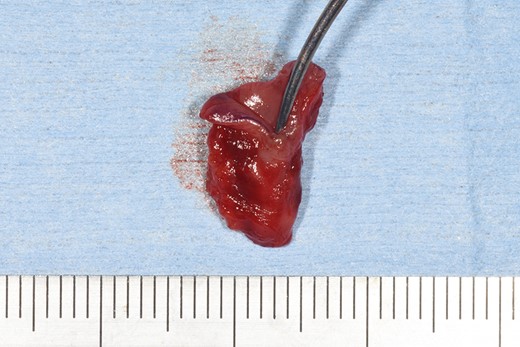
A 66-year-old man was referred to our institution in January 2018 for the diagnosis and treatment of a right buccal lesion. The lesion was first noticed approximately 1 month previously during an examination by his family dentist. The patient’s medical and family histories were unremarkable. He had no history of trauma to the face. Physical examination revealed bruising on the skin of his right cheek (Fig. 1). In the oral cavity, a mucosal outpouching (5-mm diameter, 10-mm depth) was observed in his right cheek. Food debris was seen in the outpouching (Fig. 2). The adjacent overlying oral mucosa was normal in appearance. The clinical diagnosis was a diverticulum-like lesion of the buccal mucosa. Excision of the outpouching was performed through an intraoral incision to stop food impaction (Fig. 3). It was easily separated from the surrounding soft tissues and completely excised (Fig. 4). The bottom of the outpouching was over the buccinator muscle on the lateral side. The buccinator muscle layer and oral mucosal layer were sutured separately. Histopathological examination revealed that the excised lesion was a true diverticular structure composed of a keratinising, squamous epithelial lining with a surrounding fibrous connective tissue wall, with inflammatory cell infiltration and haemorrhage (Fig. 5). In contrast to the normal buccal mucous epithelium, the diverticular epithelium had a thick stratum spinosum appearance with formation of anastomosed rete ridges (Fig. 6). The surface of the parakeratinised epithelium was corrugated. The histopathological diagnosis was a diverticulum of buccal region. The postoperative course was uneventful.


Intraoral photograph showing a pouch on the right buccal mucosa.


Histopathologic findings of the lesion revealed a true diverticulum composed of an inner layer of squamous epithelium and an outer layer of fibrous connective tissue (haematoxylin–eosin stain, ×5).
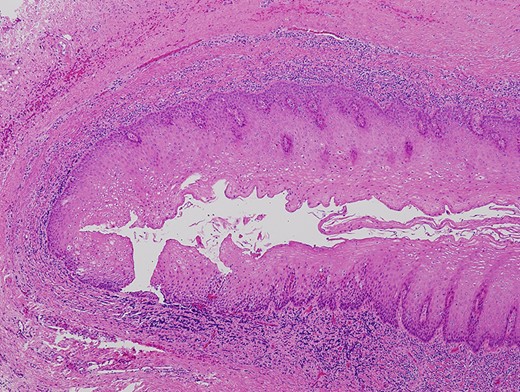
Diverticular epithelium showing a thick stratum spinosum appearance with formation of anastomosed short and broad rete ridges and a corrugated epithelial surface (haematoxylin–eosin stain, ×40).
DISCUSSION
Oral diverticula are exclusively located on the buccal mucosa of older adults. Except for one large diverticulum reported by Bailey [3], oral diverticula are relatively small (≤15 mm in both diameter and depth). Clinical symptoms of an oral diverticulum include swelling [3], halitosis [5, 7], bleeding [3], and food impaction [7]. Three reported cases [4–6] were followed up with conservative treatment, and surgical excision was performed in another three cases [3, 7, 8]. The aim of the surgery was to stop food impaction into the diverticulum [7, 8]. In the present case, surgical resection was selected for the same reason. Histopathologically, the diverticular epithelium showed a corrugated surface layer and rete ridge formation. Such histologic architecture may suggest that the diverticular mucosa is able to expand. Inflammatory cell infiltration and haemorrhage were observed under the epithelium. These findings have not been documented in the English-language literature to date. However, bleeding has been reported as a clinical symptom of oral diverticulum [3]. In the present case, bruising on the skin of the right cheek and histopathological findings of chronic inflammation suggested the occurrence of subepithelial bleeding under the outpouching.
Adequate treatment of an oral diverticulum without marked symptoms involves conservative irrigation. However, enlarging of the diverticulum during follow-up has been reported [3]. Therefore, patients should be monitored for enlargement of the outpouching when conservative treatment is selected.
In conclusion, we have reported a rare case of oral diverticulum and described its histological findings. Clinicians should be aware of this lesion to ensure correct diagnosis and treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKOWLEDGEMENTS
We thank Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.



