-
PDF
- Split View
-
Views
-
Cite
Cite
Chrisostomos Sofoudis, Dimitra Vasileiadou, Dimitrios Fagkrezos, Michael Lenos, Eythimios Papamargaritis, Andreas Gerolymatos, Necrotized torsion of enormous bilateral borderline tumors in young patient, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz168, https://doi.org/10.1093/jscr/rjz168
Close - Share Icon Share
Abstract
Borderline ovarian tumors, or tumors of low malignant potential, are neoplasms of good prognosis that affect mostly patients of reproductive age. They account for 15% of all epithelial ovarian neoplasms and they are managed with surgical cytoreduction. Conservative surgery may be considered in patients who desire fertility preservation. Here we report on a patient who presented with vague abdominal symptoms and was diagnosed with large bilateral borderline tumors, of 18 and 15 cm in size. She underwent a total abdominal hysterectomy, bilateral salpingo-oophorectomy and epiplectomy and received adjuvant chemotherapy. Borderline ovarian tumors are a pathologic entity the gynaecologist should be well acquainted with.
INTRODUCTION
Borderline ovarian tumors are neoplasms of higher proliferative activity than benign tumors, but they do not show stromal invasion, distinguishing them from invasive carcinomas [1]. Borderline tumors tend to affect a younger population and constitute 15% of all epithelial tumors of the ovary. The prognosis of borderline ovarian tumors is extremely good, with a 10‐year survival of about 95%. Early stage, serous histology, and younger age at diagnosis are associated with a more favorable prognosis [2]. The majority are of the serous subtype. Compared to mucinous, serous neoplasms are more commonly bilateral, reported in about 20–30% of cases [1, 3]. The prognosis for bilateral involvement is less favorable [4]. Approximately 65–70% of serous tumors and 90% of mucinous tumors are stage I, and 30% and 10%, respectively, are associated with extra-ovarian spread [5]. Preoperative investigations include serum tumor markers (such as CA-125) and imaging studies. Abnormal concentrations of CA-125 have been reported in about 40% of patients with stage I borderline neoplasms [6]. Besides transvaginal ultrasound, color Doppler studies and magnetic resonance imaging (MRI) can help differentiate between benign and malignant tumors [1]. The treatment consists of primary surgical staging and cytoreduction. Patients who desire fertility preservation may undergo a partial oophorectomy or cystectomy. Adjuvant chemotherapy and/or hormonal therapy are sometimes considered, mainly to prevent disease recurrence. [2]
CASE
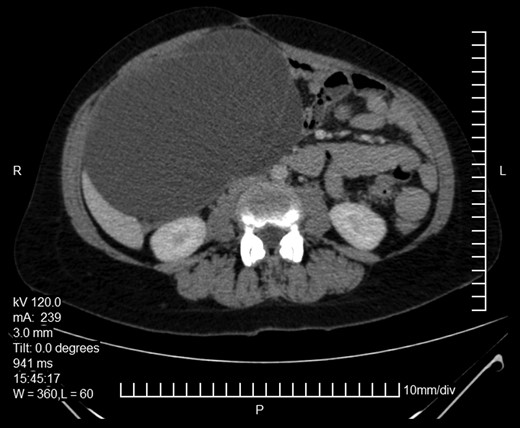
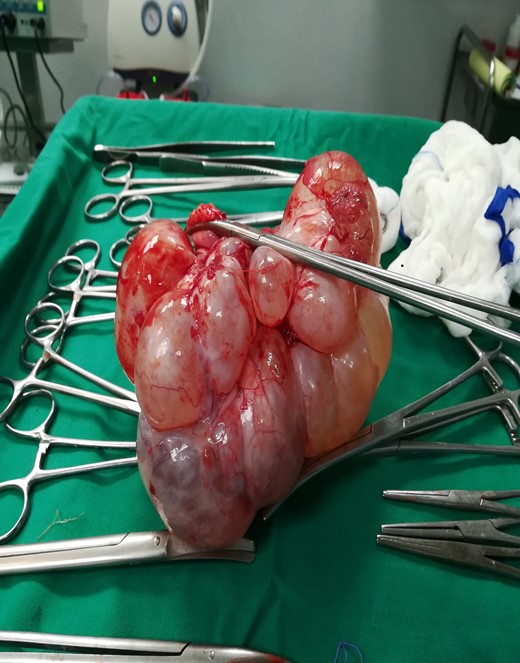
Here we report on a 32-year-old patient who presented at the Emergency Department complaining of acute abdominal pain accompanied by vomiting and diarrhea that had started three hours before. The patient was a para 2 and the latter delivery had occurred nine months before. She had been breastfeeding until 20 days before her ED visit and her menses had not yet resumed. Her medical history was unsignificant and she reported a laparoscopic ovarian cystectomy five years before, of which the histology report was not retrieved. She also had an ultrasound six months before, which described a pelvic multilocular cystic lesion of 11.4 × 8,6 × 12.3 centimeters, which remained untreated. The patient underwent an IV contrast—enhanced abdominal CT which demonstrated sizeable multilocular bilateral ovarian cystic lesions, of 18 cm and 15 cm in dimensions (in the right and left ovary respectively). (Figs 1 and 2). Her tumor markers were as follows (normal values are in parentheses): CA 15.3 = 20.53 U/ml (<25 U/ml), AFP = 1.08 ng/ml (<7 ng/ml), CEA = 0.63 ng/ml (<3.8 ng/ml), CA 125 = 110.40 U/ml (<35 U/ml), CA 19.9 = 50.06 (<34 U/ml), CA 72.4 = 6.74 (<6.9 U/ml). After the completion of preoperative investigations, the patient underwent and exploratory laparotomy. Frozen section revealed bilateral serous borderline tumors, therefore the patient underwent a total abdominal hysterectomy/bilateral salpingoophorectomy and epiplectomy. During surgical procedure astonishing remarks was the necrotized torsion of ovarian masses mimicking infiltrated ovarian neoplasm. (Figs 3–5). The final histology report confirmed the diagnosis of bilateral serous borderline tumors/atypical serous proliferative tumors, staged as pT1cNxMx or FIGO Ic. (Figs 6 and 7). Peritoneal fluid cytology showed mesothelial reactive lesions. The patient’s postoperative course was uneventful. The Multidisciplinary Team Meeting decided on adjuvant chemotherapy (four cycles of CarboTaxol; paclitaxel and carboplatin). Nine months after surgery, the patient remains alive and disease – free.
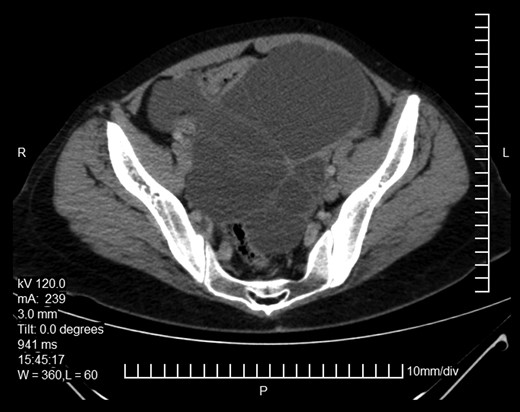
Abdominopelvic CT. Bilateral ovarian masses with characteristic diaphragms.
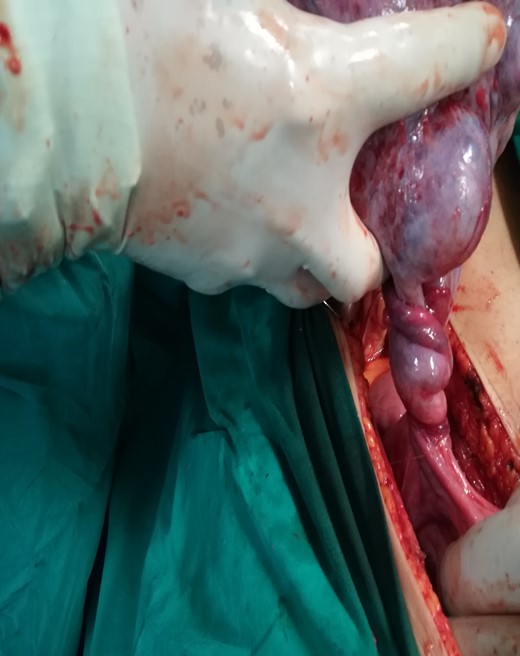
Intraoperative findings. Multilobular borderline ovarian mass.

Intraoperative findings. Multilobular borderline ovarian masss.
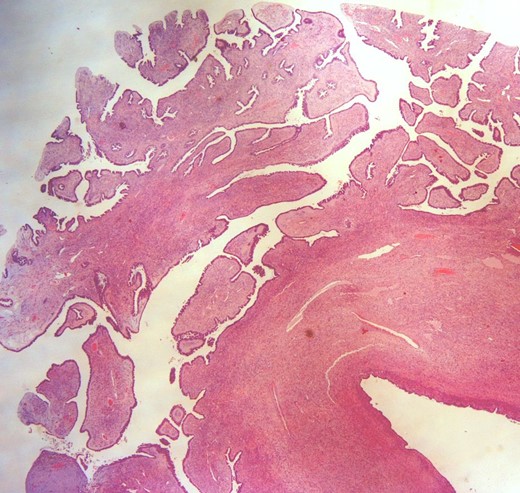
Intersection where the extrusion component is shown (H&E × 20).
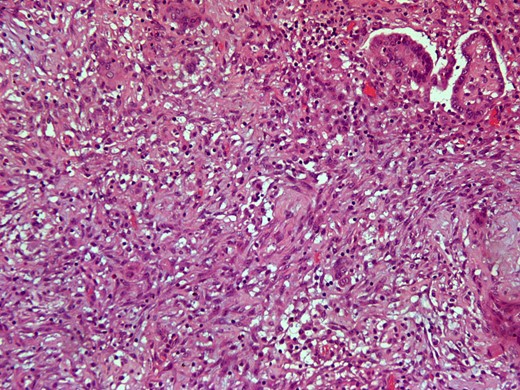
Intersection of demoplastic non-invasive autoimplantation / auto implant. (H&E × 200).
DISCUSSION
Borderline ovarian tumors are neoplasms of the reproductive age and are associated with a favorable prognosis. Our patient was diagnosed with the neoplasms soon after she gave birth, and the tumors continued to grow rapidly while she was lactating. Cases of borderline tumors in pregnant patients have been reported in the literature, [7] however it is known that increasing parity and lactation duration are protective factors for epithelial neoplasms [8, 9]. Moreover, it is quite possible that the patient had the tumors while still pregnant, but perhaps their small size then and the bulk of the gravid uterus did not allow for an accurate diagnosis. However, it has been found that ultrasound studies have a good sensitivity and specificity for the diagnosis of adnexal masses in pregnancy [10]. Finally, it is worth mentioning that while chemotherapy is usually reserved for high-risk patients or patients with recurrent disease, [2] it was decided that our patient receive adjuvant treatment on the basis of her bilateral disease and rapid growth of the masses.
CONCLUSION
Borderline tumors represent a rare entity with increased proliferative activity without ovarian stroma invasion and infiltration. Ultimate scope in such cases remains conservative surgical approach and fertility preservation in reproductive female patients.
CONFLICT OF INTEREST STATEMENT
All authors declare any financial demand with respect to the following manuscript.



