-
PDF
- Split View
-
Views
-
Cite
Cite
Kirsten Jie Ying Ong, Alexander Shaw, Richard Wadsworth, Steven Ball, Rageb Hasan, Titus Augustine, Single stage hand assisted laparoscopic and trans thoracic excision of multifocal paraaortic and cardiac paragangliomas, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz169, https://doi.org/10.1093/jscr/rjz169
Close - Share Icon Share
Abstract
A 26-year-old male, with a family history of Paraganglioma Syndrome 4 (PGL4) presented with an 18-month history of paroxysmal headaches, a one-month history of frequent diaphoresis, anxiety attacks and unintentional weight loss of one stone in 2 months. Physical examination and vital parameters were normal. Laboratory studies showed significant elevation of plasma normetanephrines and 3-methoxytyramine while DNA molecular analysis confirmed pathogenic mutation in the SDHB gene and genetic transmission of PGL4. Imaging studies demonstrated a left para-aortic mass in the mid-abdomen and a mediastinal paraganglioma between the root of aorta and origin of the main pulmonary artery, encroaching the right ventricle. After adequate alpha blockade, the patient underwent a combined sequential hand-assisted laparoscopic resection of the abdominal tumour followed by midline sternotomy and resection of the second lesion at the root of the aorta, complicated by the need for emergency cardiopulmonary bypass due to perforation of right ventricular wall.
INTRODUCTION
Paraganglioma Syndrome 4 (PGL4) is a hereditary condition which is diagnosed based on biochemical and genetic testing. In these patients, multifocal disease is seldom a feature and its presence requires experienced surgical and anaesthetic management. Despite multi-disciplinary planning, certain intra-operative challenges remain, including that of severe hypotension, sympathetic surges and associated arrhythmias. Surgery is particularly indicated in PGL4 due to a high risk of malignant transformation.
CASE REPORT
A 26-year-old male, with a family history of PGL4, presented with an 18-month history of paroxysmal headaches, a one-month history of frequent diaphoresis, anxiety attacks and unintentional weight loss of one stone in two months. His father and brother had previously been diagnosed with PGL4 and had undergone surgical resections for abdominal and pelvic paragangliomas. He underwent biochemical and genetic work-up confirming significantly elevated plasma normetanephrines and 3-methoxytyramines, with normal plasma metadrenaline levels. Full body CT, MR (Fig. 1) and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) CT imaging (Fig. 2) revealed a left para-aortic mass in the mid abdomen and a mediastinal lesion located between the root of aorta and origin of the main pulmonary artery, encroaching the right ventricle.
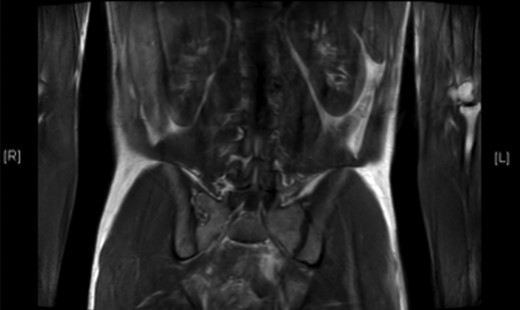
T2-weighted MRI scan showing hyper-intense mass lying anterolateral to left side of aorta in mid-abdomen.

FDG-PET scan showing 3.8 × 2.6 × 5.5 cm highly FDS avid lesion between root of aorta and origin of pulmonary artery.
Pre-operative alpha-blockade with phenoxybenzamine was titrated to a dose of 50 mg. Beta blockade was not commenced to the absence of reflex tachycardia, normal plasma metadrenalines and a resting heart rate of 60.
The patient underwent single-stage hand-assisted laparoscopic removal of the abdominal para-aortic tumour followed by sternotomy for the mediastinal mass. Handling of the abdominal tumour caused tachyarrhythmia and thus short boluses of 30 mg esmolol, an ultrashort-acting selective beta1-adrenergic blocker, was given. Intra-operatively, both lesions were noted to be hypervascular making dissection challenging. Ligation of the venous drainage of the abdominal tumour would typically cause severe hypotension and norepinephrine would be required to control the blood pressure. However, as this patient had a second catecholamine secreting tumour in his chest, there was only a slight fall in systolic blood pressure from 120 mmHg to 90 mmHg.
Pre-operative planning suggested thoracic dissection was technically feasible without cardiac bypass. However, during resection of the tumour, it was found to be densely adherent to the right ventricular surface in the aorto-pulmonary window (Fig. 3). Tumour excision caused a ventricular perforation with bleeding controlled by digital pressure. To minimize haemorrhage from the ventricular perforation and to fully excise the tumour from the origin of the right coronary artery, cardiopulmonary bypass was rapidly instituted and maintained for 44 minutes. After commencing the bypass, the patient’s blood pressure dropped rapidly from 80/40 mmHg to 30/20 mmHg. Large doses of norepinephrine, phenylephrine and metaraminol were administered to improve hypotension and pump pressure, but there was little effect due the catecholamine resistance from phenoxybenzamine alpha blockade. Adrenaline and fluids were then given and the blood pressure eventually responded and stabilized. Thereafter, the thoracic component of the tumour was successfully fully excised.
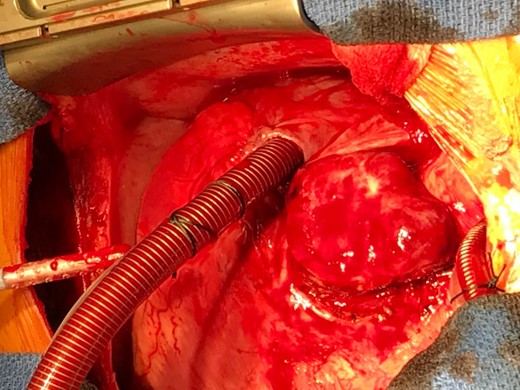
Macroscopic appearance of the specimen, showing a large, well defined and highly vascular tumour located at the aorto-pulmonary window.
Following surgery, the patient was transferred to the cardiac intensive care unit (CICU) for continuous haemodynamic monitoring and intravenous vasopressors. Blood glucose levels were also monitored closely for the first 24 hours for hypoglycaemia, which could occur due to rebound increase in insulin secretion given there is no longer excessive catecholamine inhibition of insulin secretion by the paragangliomas. He was extubated after four hours and transferred to a general ward after 48 hours. His blood pressure normalized and his heart rate was stable through his stay. He was subsequently discharged well after seven days. He remains well, two years after the procedure.
DISCUSSION
PGL4 is associated with mutations in the SDHB at gene locus 1.p36.1–35. As with other familial paraganglioma syndromes, it follows an autosomal dominant trait of inheritance and is the second most common type of familial paraganglioma after SDHD mutation [1–3]. A meta-analysis of 378 patients with SDHB tumours showed that paragangliomas were more common with 78% of patients having paragangliomas compared to 25% with pheochromocytomas. Out of the 78% with paragangliomas, 71% were reported to be sympathetic while 24% were parasympathetic. 21% presented with multi-focal lesions [4].
PGL4-related tumours are also generally associated with higher morbidity and mortality compared to the rest of the familial paraganglioma syndromes due to its higher malignant potential [3]. The excessive production of norepinephrine by sympathetic paragangliomas results in symptoms similar to its adrenal counterpart. This includes paroxysmal headaches, palpitations and excess sweating as evident in this patient. On the contrary, dopamine-secreting paragangliomas occasionally seen in patients with PGL4 often present later with mass effects and non-specific symptoms. Pre-operatively, alpha blockade should be commenced at least 2 weeks before surgery and must precede beta blockade, otherwise unopposed alpha stimulation can result in malignant hypertension. The dose of phenoxybenzamine is titrated to clinical effect to protect the patient from catecholamine storm during surgery. Historically, surgical mortality has reduced from around 40% to less than 3% following this approach [5]. Other short-acting selective alpha1-adrenergic blockers such as doxazosin and prazosin can be used with the advantage of a lower incidence of postoperative hypotension. Calcium channel blockers can be used if the patient is intolerant to alpha blockade and is especially useful in normotensive patients who develop episodes of paroxysmal hypertension. Intraoperatively, invasive haemodynamic monitoring is mandatory using arterial and central lines, coupled with good peripheral intravenous access to administer drugs efficiently in response to both catecholamine surge and deficit [7].
The management of these rare multifocal endocrine secretory tumours has the best outcomes in tertiary referral centres with specific multidisciplinary expertise to deliver a comprehensive therapeutic plan. Multiple lesions may straddle different specialities and preoperative planning and coordination are critical in achieving the best patient outcomes [6]. Minimally invasive surgery is increasingly utilized for phaeochromocytomas and paragangliomas [8]. In our case, the technique of hand assisted laparoscopic excision was effective without any significant hypertensive surges on handling the abdominal lesion. Due to the position of the thoracic lesion, a thoracotomy had to be used for access and excision. However both lesions were fully excised in one sitting with the abdominal component followed by the thoracic component with a short inpatient stay.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
SE C, WF Y. Paragangliomas: epidemiology, clinical presentation, diagnosis, and histology. Uptodate.
- anxiety
- aorta
- cardiopulmonary bypass
- pulmonary artery
- mutation
- right ventricle
- weight reduction
- physical examination
- headache
- abdominal neoplasms
- calculi
- dna
- genes
- laboratory techniques and procedures
- laparoscopy
- paraganglioma
- parity
- plasma
- abdomen
- diagnostic imaging
- heart
- hyperhidrosis
- mediastinum
- genetic inheritance
- excision
- supraaortic valve area
- ventricular wall



