-
PDF
- Split View
-
Views
-
Cite
Cite
Alan I Smith, Terry R Went, David Gaskin, Christopher A Maynard, Charles N Edwards, Atypical lipomatous tumour of the oesophagus, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz192, https://doi.org/10.1093/jscr/rjz192
Close - Share Icon Share
Abstract
Atypical lipomatous tumours (ALT) of the oesophagus are rare malignant tumours that are found most commonly in the cervical oesophagus. They are commonly misdiagnosed as giant fibrovascular polyps of the oesophagus (GFP). The differentiation between these clinical entities is important as ALTs are malignant tumours with the potential for local recurrence and metastases. We present a case of an ALT which was misdiagnosed as a GFP. The correct diagnosis was made on histological examination of the resected specimen, and confirmed by immunohistochemistry. The tumour cells extended to involve the resection margins, highlighting the need to consider this diagnosis when dealing with all oesophageal polyps, and ensure complete resection of these tumours.
INTRODUCTION
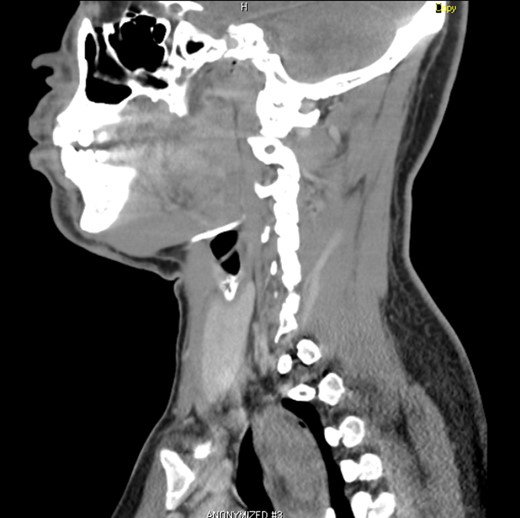
Atypical lipomatous tumours (ALT) of the oesophagus are rare malignant tumours that are found most commonly in the cervical oesophagus, and may also be termed well differentiated liposarcomas of the oesophagus. These tumours are commonly clinically misdiagnosed as giant fibrovascular polyps (GFP) of the oesophagus, and only histological examination and immunohistochemistry (IHC) reveal the true diagnosis. The differentiation between these two entities is of clinical importance as GFPs are benign whilst ALTs are malignant tumours which need to be completely excised. We present a case of an ALT which was characterized on computed tomography (CT) and upper gastrointestinal endoscopy as a GFP. The diagnosis of ALT was made on routine histology after surgical resection, and supported by IHC, highlighting the need to treat all large cervical oesophageal polyps as malignant tumours, and ensure complete resection with clear margins (Figs 1–3).
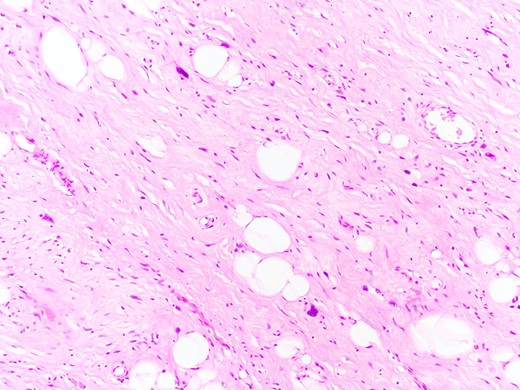
Atypical lipomatous tumour of the oesophagus with the characteristic scattered cells with large hyperchromatic nuclei (H&E, x 400).
CASE REPORT
A 37-year-old male coughed up a large mass into the back of his mouth while swallowing. He pushed the mass back down his throat and he sought medical attention following this episode. He has chronic depression and smoked a pack of cigarettes a week for thirteen years but stopped smoking a year prior to presentation. A barium swallow was done which was reported as either an ‘… oesophageal duplication cyst of the cervical oesophagus … or less likely a polyp.’ A CT scan confirmed an intraluminal cervicothoracic oesophageal lesion consistent with a large fibrovascular polyp. He then underwent upper gastrointestinal endoscopy which confirmed a large mass on a stalk extending from the cervical oesophagus to 30 cm into the oesophagus. He was then referred for surgical resection. Clinical examination identified a Grade II/VI systolic murmur. Echocardiogram showed mild tricuspid, mitral and pulmonary regurgitation with mitral valve prolapse and a small secundum atrial septal defect. A preoperative diagnosis of a giant fibrovascular polyp (GFP) of the oesophagus was made, and the patient was scheduled for surgical excision.
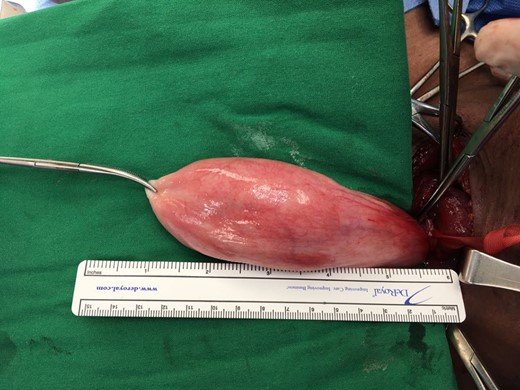
Under general anaesthesia, he underwent resection of the oesophageal polyp. An incision along the anterior border of the left sternocleidomastoid muscle was made. An enlarged left lobe of the thyroid was mobilized and retracted medially, and the sternothyroid muscle was partially divided. The cervical oesophagus was dissected out circumferentially and encircled with Nylon tape. A longitudinal 6 cm full thickness oesophagotomy was made on the left lateral aspect of the oesophagus. The polyp was identified and delivered into the wound through gentle traction. The polyp measured 14 cm in length and 3 cm in diameter. The polyp stalk was excised down to the submucosa at its point of attachment to the proximal cervical oesophagus. The oesophagus was closed in two layers with absorbable sutures. He had an uneventful post-operative course and was discharged home after a swallow with water soluble contrast showed no leak on postoperative day seven. He developed hoarseness post-operatively, and indirect laryngoscopy 3 weeks post-operatively showed paralysis of his left vocal cord. This resolved with speech therapy over the following 6 weeks.
The histology report showed a polypoid lesion with a core of fibrovascular connective tissue surmounted by unremarkable stratified squamous epithelium. Scattered cells with large irregular hyperchromatic nuclei were noted throughout, including sections from the resection margin. The specimen was sent for immunohistochemical staining and was positive for CD34 and CDK4. The final diagnosis being of an atypical lipomatous tumour of the oesophagus. Repeat upper gastrointestinal endoscopy performed fourteen months post surgery was completely normal, with no evidence of recurrence.
DISCUSSION
Giant fibrovascular polyps (GFP) of the oesophagus are uncommon, and represent nonneoplastic lesions, characterized by the presence of squamous mucosa, and containing fibrous tissue and fat. The term was first coined by Stout and Lattes in 1957 [1]. The first case of a primary oesophageal liposarcoma was reported by Mansour et al. in 1983 [2]. There have been several case reports in the literature, with the largest series being reported by Levine et al. in 1996 [3]. A recent review by Graham et al., where they looked at all the case coded as GFPs, lipomas or liposarcomas at their institution over a twenty year study period, found that all five of the cases thought to be GFPs were actually well differentiated liposarcomas by fluorescence in situ hybridization (FISH) for MDM2 [4]. They questioned whether GFPs are actually all oesophageal liposarcomas, and that at the very least the diagnosis of a GFP should only be made after careful histological examination and immunohistochemical study.
Oesophageal liposarcomas can be divided into dedifferentiated, well differentiated, pleomorphic and myxoid types. The clinical presentation of these polypoid oesophageal tumours ranges from dysphagia to regurgitation of a mass and even includes asphyxiation. Oesophageal liposarcomas carry a risk of local recurrence, and in cases of dedifferentiated type, metastases. Although no guidelines exist due to the rarity of this entity, complete resection with clear margins has to be the goal. Given the positive resection margins in our case, the patient will undergo yearly upper gastrointestinal endoscopy as surveillance for recurrence. As the diagnosis of an atypical lipomatous tumour was not entertained pre-operatively, no frozen section analysis of the resection margins was done at the time of surgery. Endoscopic resection of these lesions has also been described, and is an alternative to the open surgical resection performed in this case, however this is not available at our institution [5–7].
CONCLUSION
Atypical lipomatous tumours of the oesophagus although rare, must be considered a likely diagnosis in all cases of large oesophageal polyps. Complete surgical resection, either by endoscopic or the open route, with frozen section examination of the resection margins seems to be the most reasonable approach to these tumours. The diagnosis of a GFP should only be made after histological examination and immunohistochemical testing of the specimen.
ACKNOWLEDGEMENTS
Dr. Mehrdad Nadji, Professor and Vice Chair, Pathology, Sylvester Comprehensive Cancer Center, University of Miami Health System who performed the immunohistochemistry for the case.
CONFLICT OF INTEREST STATEMENT
None declared.



