-
PDF
- Split View
-
Views
-
Cite
Cite
Georgios Tsakotos, Anastasios Tokis, Konstantinos Vlasis, Theano Demesticha, Panagiotis Skandalakis, Dimitrios Filippou, Maria Piagkou, Arthroscopic resection of extra-articular knee osteochondroma: report of two cases, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz167, https://doi.org/10.1093/jscr/rjz167
Close - Share Icon Share
Abstract
Osteochondroma is the most common benign tumor of the growing bone, usually affecting the knee joint, located extra-articularly. Solitary intra-articular osteochondroma is very rare. In the current paper, two cases of solitary extra-articular knee osteochondromas adjacent to the capsule producing pain and restriction of knee motion are described. Diagnostic evaluation is based on combination of radiography and magnetic resonance imaging. Both osteochondromas excised arthroscopically, resulting in complete symptoms relief and full range of knee motion. On follow-up, no recurrence was recorded. Based on our experience, although limited, not only the intra-articular, but also some solitary extra-articular knee osteochondromas can be successfully treated by arthroscopy, resulting in better cosmetic result, less postoperative pain and faster recovery.
INTRODUCTION
Osteochondroma is the commonest benign bone tumor. It is likely developmental malformation rather than a true neoplasm, usually developing within the periosteum as small cartilaginous nodule [1]. Usually, the tumor is asymptomatic and located extra-articularly in the proximal femur or humerus. Osteochondromas commonly involve the knee joint, in para-articular location. Intra-articular osteochondromas of the hip and the ankle joint are very rare [2].
Hereditary multiple osteochondromas is a relatively rare autosomal skeletal dominant disorder with a prevalence of 1:50 000 persons and positive family history. It has a genetic heterogeneous background caused by loss of function mutations in genes exostosin 1, 2, 3 leading to cartilage disruption and formation of two or more cartilage capped bony exostoses of the juxta-epiphyseal region of long bones [3].
Hereditary multiple osteochondromas are usually asymptomatic and do not affect life expectancy. A wide spectrum of clinical manifestations may occur, such as pain and restricted joint motion, limb deformities due to growth plate abnormal development, low stature, cosmetic deformities, arthritis, scoliosis, impingement of the adjacent tendons or spinal cord and neurovascular disorders [1, 4]. The most severe complication is malignant transformation to chondrosarcoma in 0.5–5% of the cases. In such cases, surgical excision is necessary [1, 5].
CASE REPORTS
The first case involved a 33-year old female with pain and clicking in the right knee joint when running, bending or climbing stairs during last year. Pain exacerbated after intense sport activity. The patient received non-steroid anti-inflammatory drugs for 3 months without pain relief. In clinical examination, a palpable and audible clicking at the antero-medial aspect of the distal femur was identified. Joint range of motion was painful and restricted to 110 degrees of flexion, while extension was capable.
X-rays revealed an extra-articular mass at the medial aspect of the distal femur (Fig. 1A). Magnetic resonance imaging (MRI) confirmed the radiograph findings and no meniscal and ligament rupture or chondral defects were revealed. These characteristics were consistent with osteochondroma (Fig. 1B). Under general anesthesia, a standard antero-lateral portal used to access arthroscopically the knee. Cartilage surface, cruciate ligaments and menisci were normal. The osteochondroma was located extra-articularly, at the medial supracondylar side of the distal femur. Through a supero-medial portal and by perforating the capsule and a part of a medialis vastus muscle, the extra-articular lesion was reached arthroscopically (Fig. 2A). With an osteotome, the lesion was resected and removed with a grasper through the supero-medial portal (Fig. 2B). The remaining bony surface was abraded by a motorized shaver (Fig. 2C). The exostosis had maximum dimensions 3.1 × 2.5 cm. Histopathological examination confirmed the osteochondroma diagnosis.
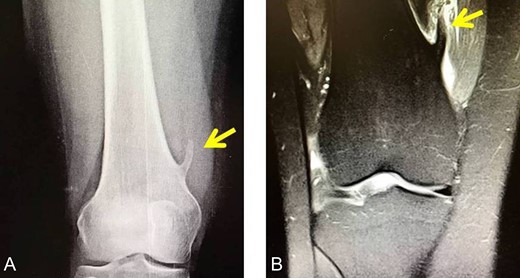
(A) The X-ray depicting the exostosis (yellow arrow), (B) MRI depiction of the exostosis.
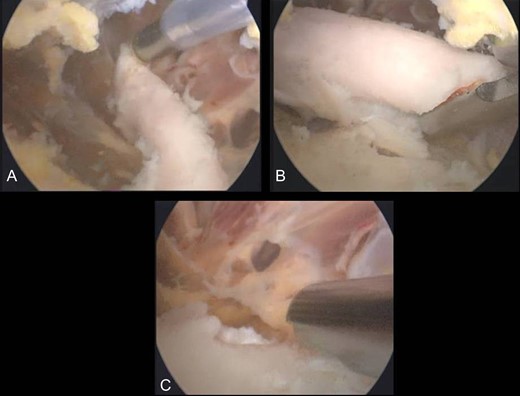
(A) Arthroscopical view of the extra-articular knee osteochondroma, (B) Arthroscopic excision of the osteochondroma, C. Abrasion of the remaining bony surface.
Postoperatively, patient was advised to use crutches for a week. Pain and clicking of knee joint eliminated immediately after surgery. The patient returned to daily activity pain free, 3 weeks after the operation. During follow-up, 3, 6 and 9 months after surgery, patient had a normal range of joint motion without pain.
The second case involved an 18 years old male with pain and swelling at the anterior surface of the left knee, under the rectus femoris muscle over the patella. Symptoms exacerbated during knee bending over 90 degrees. X-rays and MRI revealed an extra-articular exostosis, just over the suprapatellar pouch (Figs. 3A and B). Under general anesthesia, a standard antero-lateral portal was used to access the knee arthroscopically. The capsule of the suprapatellar pouch was divided providing access to the adjacent extra-articular osteochondroma. Through a medial, a far supero-medial and supero-lateral portal, the exostosis resected by using an osteotome and removed with a grasper through the supero-lateral portal. The lesion had maximum dimensions 3.1 × 1.4 cm and its histopathological examination set the diagnosis of osteochondroma. Postoperatively, the patient was pain free with full range of knee motion. No recurrence was observed at 9 months (Fig. 4).
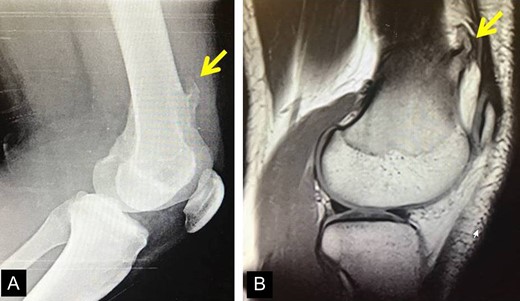
(A) X-ray of the exostosis in the second patient, (B) MRI depicts the lesion.

DISCUSSION
Extra-articular osteochondromas are the commonest benign tumors, solitary or multiple [1, 6] presented during childhood and adolescence [5]. Intra-articular osteochondromas are very rare [7, 8]. Genetic studies [9] showed a strong association between hereditary multiple osteochondromas and the loci of exostosin-1 (chromosome 8q24.1), -2 (chromosome11p13) and -3 (short arm chromosome 19).
Both extra-articular and intra-articular lesions may cause pain, discomfort and restriction of the joint motion. Differential diagnosis include synovial chondromatosis, low-grade chondrosarcoma and osteosarcoma [5, 6, 9].
Imaging plays an essential role in osteochondroma diagnosis, as it is based on preoperative X-ray and MRI findings combined with medical record and clinical symptoms. Although preoperative diagnosis may be achieved, surgical excision and histopathological examination is required to rule out malignancy, cellular atypia and mitotic activity [6–8].
Although open surgical excision is the treatment of choice for extra-articular osteochondromas and arthroscopy for intra-articular osteochondromas, most intra-articular lesions have been treated via open surgery. The open approach, near to or into the articular joint carries the risk of infection; an arthrotomy may cause joint stiffness, postoperative pain and delay to return to activity. To the best of our knowledge, no report in the literature exists concerning extra-articular knee osteochondroma resection through arthroscopy. The referred atraumatic arthroscopic osteochondroma excision may be less painful and results in a faster recovery, compared to the traditional open surgery.
In conclusion, when possible, such in the presented cases, the technically demanded arthroscopical resection of extra-articular osteochondroma offers many advantages, such as better cosmetic result, less postoperative pain and faster recovery.
CONFLICT OF INTEREST STATEMENT
The authors declared no potential conflicts of interest.
FUNDING
The authors received no financial support for this article
AUTHOR CONTRIBUTIONS
GT and AT performed the operation, KV and TD interpreted the data and DF, PS and MP participated in conceiving the study design and revising the manuscript. All authors had read and approved the final manuscript.



