-
PDF
- Split View
-
Views
-
Cite
Cite
Suman Khanal, Akash Chitrakar, Bikash Nepal, Prakash Sayami, Yogendra P Singh, Secondary angiosarcoma in a hormone receptor negative breast cancer patient, Journal of Surgical Case Reports, Volume 2019, Issue 6, June 2019, rjz166, https://doi.org/10.1093/jscr/rjz166
Close - Share Icon Share
Abstract
Post-irradiation angiosarcoma arising in the irradiated breast after breast‐conserving surgery is uncommon though being reported with increasing frequency. Such cases are reported mainly in hormone-receptor positive patients who had received hormonal therapy along with radiation. We describe a rare case of post-irradiation angiosarcoma in a 71-year-old hormone-receptor negative female who did not receive hormonal therapy.
INTRODUCTION
Angiosarcomas account for 1% of soft tissue tumors and breast angiosarcomas account for eight percent of all angiosarcomas [1]. Breast angiosarcomas may be primary or secondary. Secondary angiosarcomas are usually found in older women who have undergone breast cancer treatment with radiation. There are two types of secondary angiosarcoma: lymphedema-associated cutaneous angiosarcoma and post-irradiation angiosarcoma. The period prevalence proportion of post-irradiation angiosarcoma appears to be low at 0.16–1.11% [2].
Post-irradiation angiosarcomas are high grade, locally aggressive with high local recurrence rates, distant metastases and poor long-term survival [3]. All cases of such angiosarcomas are reported in hormone-receptor positive breast cancer patients. Here we report a case of intermediate grade angiosarcoma in a hormone-receptor negative patient.
CASE REPORT
A 71-year-old lady had undergone breast-conserving surgery (BCS) for invasive ductal carcinoma, no specific type (NST) of right breast nine years prior to current presentation in our unit. Her pathological stage at that time was T2N1M0 with negative estrogen and progesterone receptor status. She had received three cycles adjuvant chemotherapy with Epirubicin, 5-Fluorouracil and Cyclophosphamide 26 days post-operatively followed by adjuvant irradiation of the right breast with 50 Gray and again three cycles adjuvant chemotherapy with the same regimen.
She remained well after adjuvant therapy and was under regular follow up until this presentation. She presented this time with nodules in her lower inner quadrant of right breast for four months with discoloration, thickening and puckering of surrounding skin (Fig. 1). There was no palpable mass in axilla or contralateral breast and no lymphedema of right upper limb. She had diabetes mellitus, hypertension and hypothyroidism. There was no history of headache, weight loss, jaundice or back pain.

Splotchy purplish nodules in right breast in lower medial quadrant (A) With surrounding discoloration (B) Close up view.
Contrast enhanced computed tomography (CECT) of chest and abdomen showed two enhancing cutaneous nodules measuring 19 mm × 18 mm and 18 mm × 14 mm in medial aspect of right breast with minimal fat stranding noted in superficial subcutaneous plane (Fig. 2). Surrounding skin was edematous. Other findings were lobulated outline of liver and few splenic cysts with no evidence of systemic metastasis. Fine needle aspiration cytology (FNAC) from the nodule revealed clusters and fragments and singly dispersed spindle shaped cells with elongated hyperchromatic nuclei with moderate cellular pleomorphism suggestive of malignant spindle cell neoplasm.
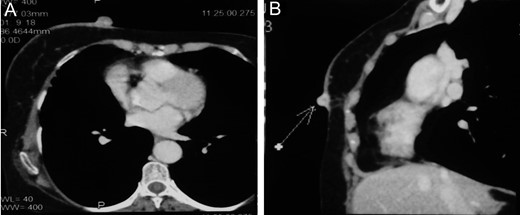
CECT showing enhancing cutaneous nodules in right breast with minimal fat stranding without evidence of deeper tissue penetration (A)Axial section (B)Sagittal section.
The patient underwent total mastectomy with negative margins. Intra-operatively there were two nodules (15 mm × 15 mm and 15 mm × 15 mm) arising from right breast skin without involving deeper tissues with thickening of surrounding skin and subcutaneous tissue (Fig. 3).

Histopathology report of the specimen showed intermediate grade angiosarcoma infiltrating into subcutaneous tissue (Fig. 4).
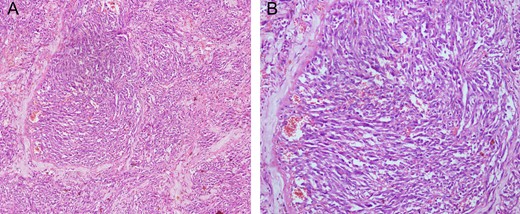
Histopathology (Hematoxylin & Eosin stain) showing interanastomosing vascular channels with cytologic atypia and infrequent mitoses suggestive of intermediate grade angiosarcoma (A) 100x magnification (B) 200x magnification.
Three months after mastectomy, the patient presented again with a splotchy purplish nodule in the right breast below the scar line which on FNAC proved to be spindle cell neoplasm. The patient was advised for wide local excision, however the patient opted for chemotherapy. Patient succumbed to progressive disease six months after the local recurrence.
DISCUSSION
Secondary post-radiation angiosarcoma without lymphedema was reported first in 1981 [4]. Secondary angiosarcoma tends to involve the subcutaneous tissues of the breast, while sparing the underlying breast parenchyma.
The relative risk of developing angiosarcoma in irradiated breast is increased by 16-fold [5]. Clinical presentation is diverse with lesions often described as erythematous or violaceous nodules, plaques, or patches. The recommended way of diagnosis is suggested to be punch biopsy especially in non-palpable lesions with skin changes [2]. We opted for FNAC because our lesions were nodular.
Secondary angiosarcoma are more likely to be of high-grade (82%) compared to primary angiosarcoma [6]. Literature review shows many reports of secondary post-irradiation angiosarcoma in females to be hormone-receptor positive breast cancers under hormonal therapy [6, 7]. Our case is unique in that the angiosarcoma was of intermediate grade and occurred in hormone-receptor negative patient without any hormonal therapy.
The risk of developing secondary angiosarcoma does not outweigh the benefit of treatment so radiotherapy continues to be a mainstay modality in the treatment of breast cancer patients. Compared with the latency of other radiation-associated sarcomas, the latency for post-irradiation angiosarcoma of breast is relatively short with a median of 5.2 years [8] which in our case was 9 years. Recurrence was quite early at three months compared with 7.5 months in a study done at French Cancer Centers [9] though these centers didn’t have data on hormone receptor status. Our case succumbed early to progressive disease at nine months against the median survival of 15.5 months [9]. Resection with negative margins might not be adequate treatment for post-irradiation angiosarcoma. Recent paper published by Li et al. have found radical resection (irradiated skin and mastectomy) to be associated with reduced recurrence and improved disease free survival [10]. The recurrence and reduced survival in our case could be attributed to the residual irradiated skin, though the lesion was excised with negative margins.
CONCLUSION
As the recent trend towards BCS increases, the incidence of post-irradiation angiosarcoma is also likely to steadily increase in the future. The possibility of angiosarcoma should be routinely discussed with both hormone-receptor positive and negative patients considering breast-conserving surgery. Management of secondary angiosarcoma should also include excision of irradiated skin along with the tumor as irradiated skin may act as a nidus for recurrence.
ACKNOWLEDGMENTS
YPS planned the management. BN and PS were operating surgeons. All authors participated in the study and helped draft the manuscript. All authors read and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
All authors have no competing interests.
FUNDING
The authors received no financial support for the research and/or authorship of this article.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.



