-
PDF
- Split View
-
Views
-
Cite
Cite
Antonios Patrinos, Maria Zarokosta, John Tsiaoussis, George Noussios, Τheodoros Piperos, Menelaos Zoulamoglou, Ioannis Flessas, Theodoros Mariolis–Sapsakos, The clavipectoral fascia as the unique anatomical criteria for distinguishing breast parenchymal lesions from axillary lymph node metastasis, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz135, https://doi.org/10.1093/jscr/rjz135
Close - Share Icon Share
Abstract
Diagnosing primary breast tumors of the axillary tail of Spence may be extremely challenging, since several lesions may be located in the axillary fossa. In the presented case, a 54-year-old post-menopausal Caucasian female patient presented to our institution complaining about a lump in her left axilla. The preoperative imaging modalities could not clarify whether the tumor is part of the tail of Spence or metastasis of the axillary lymph nodes. The diagnosis of primary adenocarcinoma of the axillary tail of Spence was made during a quadrantectomy of the left breast after the clavipectoral fascia, which constitutes the sole anatomical boundary between breast and axilla, was identified.
INTRODUCTION
Diagnosing primary breast tumors of the axillary tail of Spence may be extremely challenging. Lesions located in the axillary fossa may have several clinical explanations and sometimes, physical examination and laboratory evaluation may not be sufficient enough to establish a differential diagnosis [1]. In the presented case, the diagnosis of a primary adenocarcinoma of the axillary tail of Spence was established at surgery. The presented case aims to highlight the surgical significance of the clavipectoral fascia, which constitutes the sole anatomical boundary between the breast tissue and the axilla.
CASE REPORT
A 54-year-old post-menopausal female presented to our institution with a palpable lump in her left axilla. Physical examination revealed a solid, fixed, painless mass, 3.3 cm × 2.9 cm in the left axillary fossa. There were no overlying skin abnormalities or any further abnormal clinical findings. The contralateral breast and axilla were normal.
Following these, mammography was performed but it was not helpful due to the location of the mass. The breast ultrasound (U/S) and the U/S of the axilla detected a hypoechoic mass in the axillary fossa. MRI was also conducted, confirming a single lesion in the left axilla. There were no additional lesions seen in the same or contralateral breast on MRI (Fig. 1). Subsequent core needle biopsy (FNAB) established the diagnosis of breast infiltrating ductal carcinoma (Not otherwise specified), grade 2. Based on this a decision was made to proceed to quadrantectomy.During the surgery, the tumor was detected superficial to the clavipectoral fascia (Figs 2–4). A quadrantectomy was performed along with axillary lymph node block dissection since the sentinel node was positive for metastasis. The rest of the operation continued in the usual fashion. A drain was placed at the end of the procedure. The post-operative recovery was uneventful. The patient was discharged five days after the surgery, when the drain was finally removed.
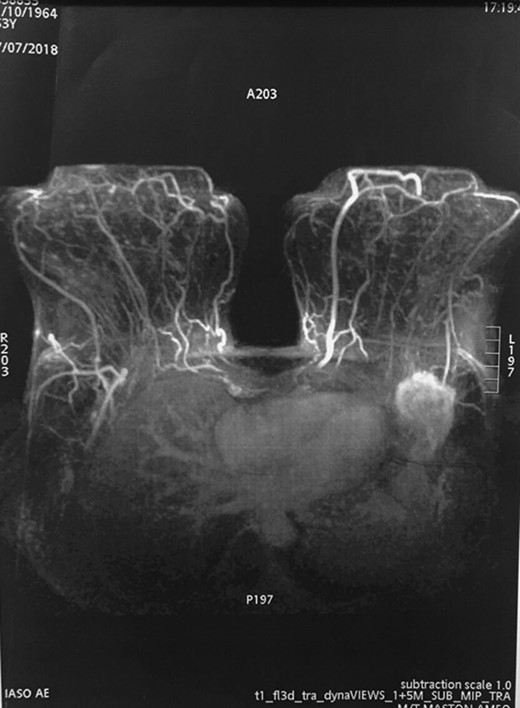
MRI detected the tumor in the left axilla. However, it cannot clarify whether the tumor is part of the tail of Spence or metastasis of the axillary lymph nodes.
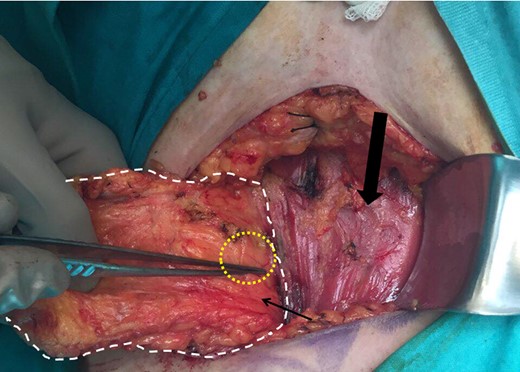
Meticulous exposure of the operating field. Yellow circle: the malignant tumor, white outline: upper external quadrant of the left breast and the left tail of Spence, thin arrow: clavipectoral fascia, thick arrow: pectoralis major.
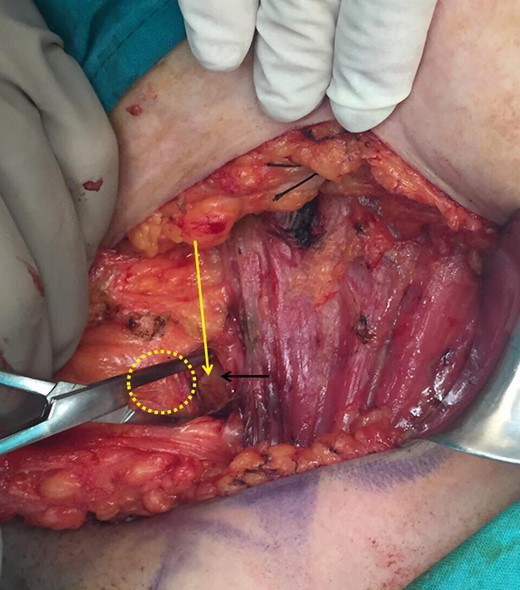
Yellow circle: the malignant tumor, black arrow: clavipectoral fascia, yellow arrow: incision of the clavipectoral fascia reveals if the mass is lymphatic or part of the axillary tail of Spence.
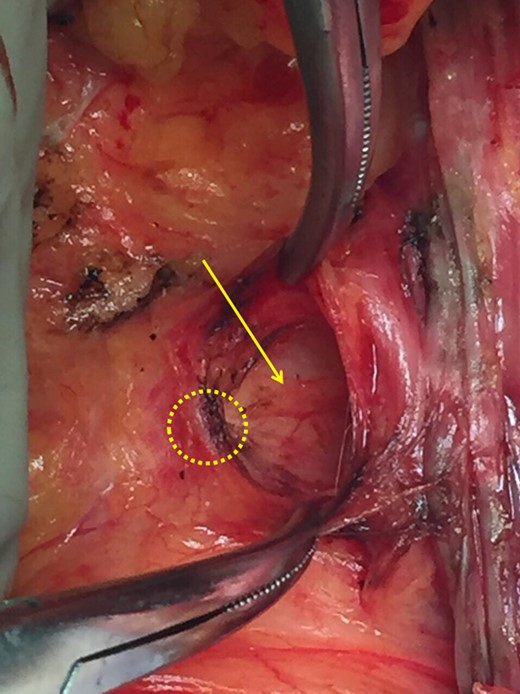
Yellow circle: the malignant tumor, black arrow: clavipectoral fascia, yellow arrow: incision of the clavipectoral fascia reveals if the mass is lymphatic or part of the axillary tail of Spence.
Further pathological examination of the tumor agreed with the pre-operative diagnosis of infiltrating ductal carcinoma in the axillary tail of Spence. Fifteen lymph nodes were dissected out of which eleven were involved with metastasis. Further immunostaining for estrogen, progesterone receptors (ER, PgR) and Her-2 was positive. The Ki-67 was 60%. The patient received adjuvant chemotherapy, Tamoxifen hormonotherapy and radiation therapy according to the oncologists’ instructions.
DISCUSSION
In cases of axillary cancerous masses physicians are called on to postulate a definite diagnosis prior to any invasive procedure. The differential diagnosis would include occult breast cancer with axillary metastasis, axillary tail breast cancer (including intramammary lymph node involvement), metastatic lymphadenopathy due to non-breast cancer and ectopic breast cancer [1].
In the presented case, neither radiology nor pathological evaluation was able to determine the exact nature of the specific tumor. Clinically ectopic breast cancer was excluded as the mass was not subcutaneous [2]. Furthermore, metastatic lymphadenopathy from a non-breast organ was ruled out by the initial biopsy results [3].
Our team was facing a diagnostic dilemma, was the lesion a primary breast cancer arising from the tail of the breast or was it a metastatic lymph node mass extending into the tail of the breast? A literature search revealed that this is not a unique situation with more than one article reporting on the topic [2, 4, 5]. MRI is the better choice when evaluating the axilla compared to other imaging modalities [1, 6].
Even though preoperative biopsies did not identify lymphatic tissue, we were not absolutely convinced that the lesion was not complete infiltration of lymph nodes by metastatic breast cancer, given the radiological findings. Destruction of the normal lymphatic structure due to complete infiltration would still give the impression of a primary breast cancer under microscopic examination.
The diagnostic question could only be answered during surgery. The mass was located superficial to the clavipectoral fascia and therefore a diagnosis of adenocarcinoma of the tail of Spence was established. Had we assumed that the patient had occult breast cancer with lymph node metastasis, she would have received neo-adjuvant chemotherapy that would have altered her stage and prognosis.
With this present case we attempt to underline the importance of the clavipectoral fascia and its diagnostic use as the sole anatomical boundary. According to our observations, any histologically confirmed axillary breast malignancy that is found superficial to the clavipectoral fascia confirms an axillary tail of Spence tumor while any mass beneath the fascia confirms axillary lymph nodes.
CONFLICT OF INTEREST STATEMENT
None declared.



