-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher Bierton, Anurag Gupta, Giant duodenal diverticulum—an incidental finding, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz120, https://doi.org/10.1093/jscr/rjz120
Close - Share Icon Share
Abstract
A 72-year-old female presented to the Emergency Department with 12 hours of non-specific epigastric pain. Her epigastrium was tender and inflammatory markers were mildly increased. A Computed Tomography scan revealed no acute pathology however there was a giant diverticulum arising from the second/third part of the duodenum measuring 9.5 × 5.7 × 7.3 cm. This was thought to be incidental, her pain settled and she was discharged. Diverticula are common throughout the gastrointestinal tract, predominantly in the colon. Within the small bowel they occur most commonly in the duodenum and are often asymptomatic and found incidentally. Potential complications of duodenal diverticula include pain, bleeding and obstruction. There are only a few cases reported of duodenal diverticula this large but it is important to be aware of them as a potential pathology and keep them and their associated complications as a differential for patients presenting with an acute abdomen.
INTRODUCTION
Duodenal diverticula are not uncommon findings and are often found incidentally. We present a case of a giant duodenal diverticulum with objective measurements as the current literature only has a handful of cases described such. Although not causing acute complications in our case, it is an important condition to consider in the setting of acute upper gastrointestinal symptoms or complications.
CASE REPORT
A 72-year-old female presented to the Emergency Department (ED) with sharp, non-radiating epigastric pain for less than 12 hours duration without aggravating factors or other associated symptoms.
She had an extensive past medical history including Wegener’s granulomatosis, chronic renal failure, primary biliary cirrhosis, chronic obstructive airways disease, ischaemic heart disease, liver haemangiomas undergoing surveillance and a hiatus hernia seen on oesophagogastroduodenoscopy (OGD). She was an active smoker and rarely drank alcohol.
On examination she was afebrile, with observations within the normal parameters. Her abdomen was tender with voluntary guarding in the epigastrium. Her initial blood tests were all normal other than mildly increased inflammatory markers. She underwent a non-contrast (due to chronic kidney disease) Computed Tomography (CT) scan that revealed no evidence of acute biliary/gallbladder disease, however there was the appearance of a large duodenal diverticulum. The patient was recalled for an oral contrast study that confirmed a giant duodenal diverticulum arising from the second/third part of the duodenum measuring 9.5 × 5.7 × 7.3 cm. There were no signs of surrounding inflammation or pending rupture and this was thought to be an incidental finding. Upper abdominal ultrasound revealed no acute biliary tract disease. Her pain settled and she was discharged home.
On retrospective analysis of prior scans (CT and Magnetic Resonance Imaging (MRI)) of this woman there was evidence of this duodenal diverticulum for over five years and previous OGD three years prior had noted two duodenal diverticula; one small and one large. The patient denied previous knowledge of these findings (Fig 1 and 2).

Axial slice of computed tomography (CT) scan—giant diverticulum with air-fluid level containing oral contrast.
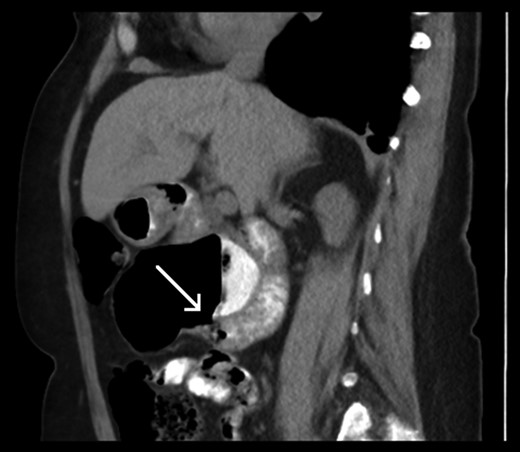
Sagittal slice of computed tomography (CT) scan—giant duodenal diverticulum partly filled with oral contrast. The arrow is indicating the neck of the diverticulum.
DISCUSSION
Diverticula are common throughout the gastrointestinal tract but are predominantly in the large colon. Within the small bowel they occur most commonly in the duodenum [1]. Often they are asymptomatic and found incidentally via various means [2]. Duodenal diverticula have previously been found in 1–5% of barium examinations [1], 7% of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) [2] and 20% of autopsies [1]. Potential symptoms and complications of duodenal diverticula include pain, bleeding and obstruction of the bowel or biliary system.
On investigation they be mistaken for abscesses with an air-fluid level or thought to be a separate loop of bowel [3]. As noted with our patient, she had multiple modalities of abdominal imaging that had not previously reported this diverticulum. Hers was thought to be asymptomatic and therefore did not need emergent management, however it should be kept in mind as a potential cause of acute abdomen in the future.
In a literature review for ‘giant duodenal diverticulum’ there were only a few cases reported and less with specific measurements of the diverticulum. Millard J et al. [1] reported four cases of giant diverticula, two that measured 11 and 10 cm at initial diagnosis and two others described as ‘large’. Horst M, et al. [4] presented a case report with a duodenal diverticulum measuring 6.8 × 4.5 × 1.8 cm with a number reporting ‘giant’ [3, 5] and ‘very large’ [2] diverticula among others.
This case was a good example of a giant duodenal diverticulum that had not previously been noted on abdominal imaging and appeared to be asymptomatic. For our patient specifically, if she continued to have non-specific abdominal pain it may be worthwhile considering the diverticula as a potential cause. As an overarching principle it is also important to be aware of duodenal diverticula as a potential pathology and keep it, with its associated complications, as a differential for patients presenting with an acute abdomen.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The corresponding author is not a recipient of a research scholarship or any other external source of funding.
CONFLICTS
There are no conflicts of interest.
DISCLOSURE STATEMENT
Signed consent from the patient involved has been obtained and the entire article including the figures has been approved by the Human Research Ethics Committee for the Central Adelaide Local Health Network.



