-
PDF
- Split View
-
Views
-
Cite
Cite
Tali Lior, Rajeev Shukla, Gavin M Wright, Excision of Giant Schwannoma in a Nonagenarian—operative techniques for enhanced recovery after thoracotomy in the high-risk patient, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz110, https://doi.org/10.1093/jscr/rjz110
Close - Share Icon Share
Abstract
Thoracotomy is acknowledged as one of the most painful procedures in surgical practice, with the potential to result in significant acute and chronic sequelae, which become especially relevant in high-risk patient populations. Certain pathologies necessitate this surgical approach, and in those circumstances we must aim to mitigate postoperative complications by employing surgical techniques that decrease the risk of nerve injury, rib fracture, and unnecessary soft tissue trauma. We describe an approach to thoracotomy that incorporates evidence-based strategies to lessen the risk of these potential complications, which resulted in rapid postoperative recovery in a nonagenarian.
INTRODUCTION
Thoracotomy is acknowledged as one of the most painful procedures in surgical practice [1]. The acute sequelae, caused by impaired deep breathing and coughing secondary to pain, include atelectasis and pulmonary infection, as well as complications associated with delayed mobility after major surgery [2]. Chronic pain after thoracotomy is reported in up to 50% of patients [3]. The elderly are at particular risk for the development of acute postoperative complications [4]. Minimally invasive thoracic surgery results in decreased rates of pulmonary complications [5], however certain pathology will necessitate an approach via thoracotomy to enable resection. To this end, multiple strategies have been proposed to minimize the pain associated with thoracotomy—we report a technique of combined surgical modifications to reduce post-operative pain secondary to nerve injury and rib fractures.
CASE REPORT
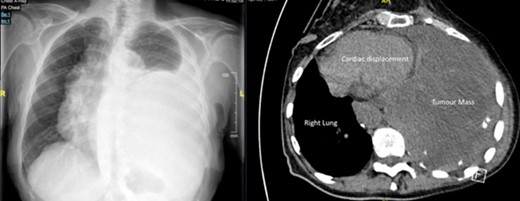
A 92-year-old, previously independent female presented acutely with severe resting dyspnoea, exercise tolerance of less than fifty metres—limited by dyspnoea and presyncope, orthopnoea, peripheral oedema and early satiety. Complete whiteout of left mid-to-lower zones with accompanying mediastinal shift was seen on initial chest X-ray (Fig 1b). CT chest performed in view of these findings demonstrated a giant (130 × 133 × 147 mm) posterior mediastinal mass arising from the left T10/T11 foramina, and causing significant cardiac displacement and complete collapse of left lower lobe and lingula (Fig 1b). Ventilation-perfusion scan showed a matched defect affecting the entire lower lobe and lingula. Percutaneous biopsy of the mass demonstrated a schwannoma (Fig 2).

The patient underwent preoperative workup and anaesthetic assessment prior to proceeding to theatre.
The patient was intubated using a single-lumen endotracheal tube with a bronchial blocker placed for left lung isolation. In the lateral decubitus position, a lateral serratus-sparing thoracotomy was performed in the sixth intercostal space. En-bloc detachment of the sixth intercostal muscle and neurovascular bundle (NVB) was performed along the thoracotomy and allowed to ‘drape’ into the pleural cavity. 1 cm of the posterior rib was resected to enable tension-free rib spreading (Fig 3). Careful bone-on-bone placement of the Finochietto retractor protected against nerve crush injury. Sufficient exposure was obtained with limited retraction. The well-encapsulated tumour was mobilized free of the posterior mediastinum and feeding vessels divided using a harmonic scalpel. The tumour was removed en-bloc in a specimen retrieval bag (Fig 4). A paravertebral catheter was placed for postoperative analgesia. A 24Fr intercostal catheter was placed prior to closure. 5 mm holes were drilled into the body of the seventh rib, through which rib approximation sutures were passed and intra-rib suturing performed – allowing tension- and compression-free rib approximation.

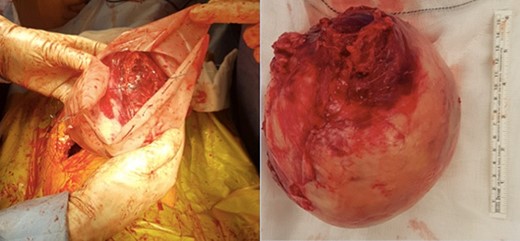
(a) Tumour extraction using specimen bag. (b) Tumour size ex-vivo.
The patient was extubated postoperatively and transferred to the ward. She recovered well, and began mobilizing on postoperative day 1. The chest drain was removed on postoperative day 2 after complete lung re-expansion (Fig 5). Paravertebral catheter was removed on postoperative day three, and the patient transitioned to oral analgesia without issue. There were no postoperative complications, and the patient was discharged home on postoperative day 4.

DISCUSSION
The potential for acute and chronic morbidity after thoracotomy is significant and well established. Certain pathologies, however, necessitate this surgical approach, and in those circumstances we must aim to mitigate postoperative complications by employing surgical techniques that decrease the risk of nerve injury, rib fracture, and unnecessary soft tissue trauma. We describe an approach to thoracotomy that incorporates evidence-based strategies to improve postoperative recovery:
Muscle-sparing incision: Serratus-sparing thoracotomy reduces degree of soft tissue trauma and allows preservation of chest wall musculature.
Neurovascular bundle detachment: Mobilization and creation of pedicle of intercostal muscle and NVB from the lower border of the rib above the breached intercostal space. This avoids potential for nerve injury during rib resection, while separation of the NVB from the rib prevents nerve crush injury due to retractor placement.
Short segment rib resection (shingling): 1 cm posterior rib resection enables sufficient access to pleural space via tension-free rib spreading, and minimizes the risk of inadvertent rib fracture and posterior ligament rupture.
Limited retraction: Judicious use of the retractor minimizes rib spreading under tension – this is enabled by the short segment rib resection.
Intra-rib suturing: Avoidance of pericostal suturing during closure prevents nerve crush injury. This is achieved by drilling 5 mm holes in the body of the rib below, through which rib approximation sutures are passed. This allows tension- and compression-free rib approximation [6].
Anatomical rib closure: ribs are only closed to their anatomical approximation in order to reduce somatic pain
We have demonstrated successful high-risk thoracic surgery in a nonagenarian by adhering to precise surgical execution of evidence-based techniques to minimize rib fracture, pain, and ultimately respiratory complications.
CONFLICT OF INTEREST STATEMENT
None declared.



