-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel A Molina, Miguel A Moyon, Fernando X Moyon, Jorge F Tufiño, Lenin J Guzmán, R Alejandro Mecias, Jaime M Cevallos, D Santiago Serrano, Subcapsular liver hematoma after extracorporeal shock wave lithotripsy, a rare complication, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz114, https://doi.org/10.1093/jscr/rjz114
Close - Share Icon Share
Abstract
Extracorporeal shock wave lithotripsy (ESLW) is a common and relatively safe procedure, with a high success rate and low adverse effects. Complications of this procedure are usually limited to the kidneys and almost always resolve spontaneously. However, on rare occasions, a frightening complication, as a hematoma of a parenchymatous organ, such as the liver can appear. Abdominal pain is usually the only manifestation when a liver hematoma develops, and should always be investigated, as this dreaded complication can put the patient’s life at risk. Conservative treatment is usually the treatment of choice, nevertheless, on severe cases that do not respond to conservative measures, surgery or embolization is necessary. We report the case of a 38-year-old male who underwent ESWL, 12 h after the procedure he presented to the emergency room with severe abdominal pain, after complementary exams a liver hematoma was detected. Following conservative management, the patient fully recovered.
INTRODUCTION
Urolithiasis is a major clinical and economic burden for the healthcare system and extracorporeal shock wave lithotrips (ESWL) has become a reliable therapy, mostly due to its high success rate and low adverse effects [1, 2]. However, on certain occasions, a life-threatening complication such as a hepatic hematoma can occur [3]. Treatment is usually based on constant surveillance and supportive measures, nonetheless, surgery or embolization should be performed on severe cases. [1, 4] We report the case of a 38-year-old who developed a hepatic hematoma after ESWL, following conservative management patient underwent full recovery.
CASE REPORT
A 38-year-old male with a past medical history of right inguinal hernia, presented to the emergency room with a 10-day history of right flank pain. His pain came in waves and fluctuated in intensity throughout the day, in the last 24 h prior to admittance his pain became more intense and was followed by recurrent episodes of severe vomiting.
On clinical examination, a dehydrated and tachycardic patient was encountered. He had pain in his right flank that radiated to his lower abdomen and groin. Complete blood count (CBC) and urinalysis appeared normal, however, an abdominal computed tomography (CT) detected bilateral nephrolithiasis, multiple 5 mm, and 6 mm lesions were identified on both the right and left kidney. Also, a 7 mm hyperdense shadow in the middle of the right ureter that caused proximal hydronephrosis was detected as well (Fig. 1A and B).
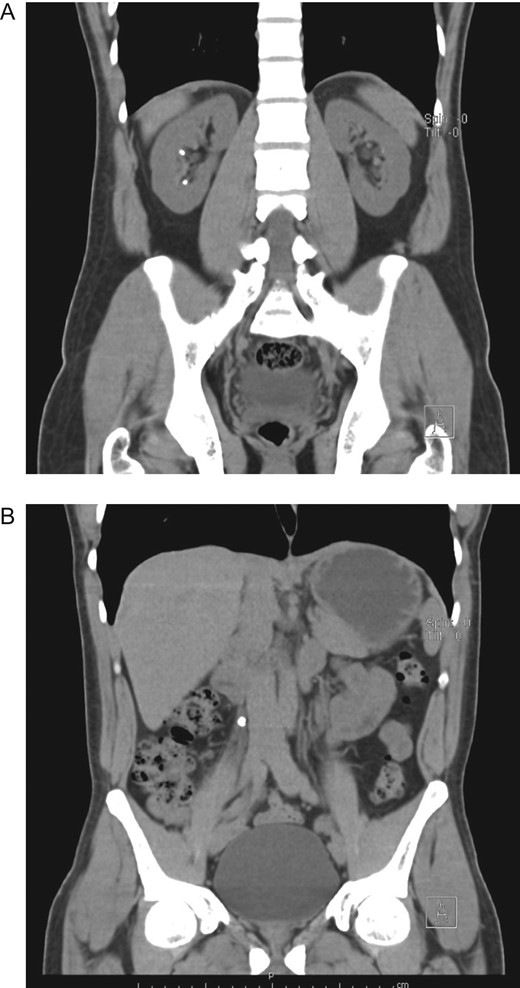
(A) CT, revealing bilateral nephrolithiasis. (B) CT, with a 7 mm hyperdense shadow in the middle of the right ureter.
Urologist consultation was required and he underwent ureteroscopic lithotripsy without complications, the ureteral stone was removed and a right double J-stent was placed. Afterward, ESWL was decided for the right nephrolithiasis. A total of 3000 shocks were delivered at a maximum power of 15 kV and a rate of 80 shocks per minute. After the therapy was completed, the patient was discharged without any apparent complication. Nonetheless, 12 h after ESWL, severe pain appeared in his right flank, thus he presented to the emergency room. On clinical examination, a dehydrated, tachycardic and hypotensive patient was encountered. Pain was discovered on his right flank without tenderness. A contrast-enhanced abdominal CT revealed a 9 × 6 × 4 cm3 subcapsular liver hematoma, with an estimated volume of 300 ml that involved almost the entire right liver, without an active contrast material extravasation (Fig. 2A–C).
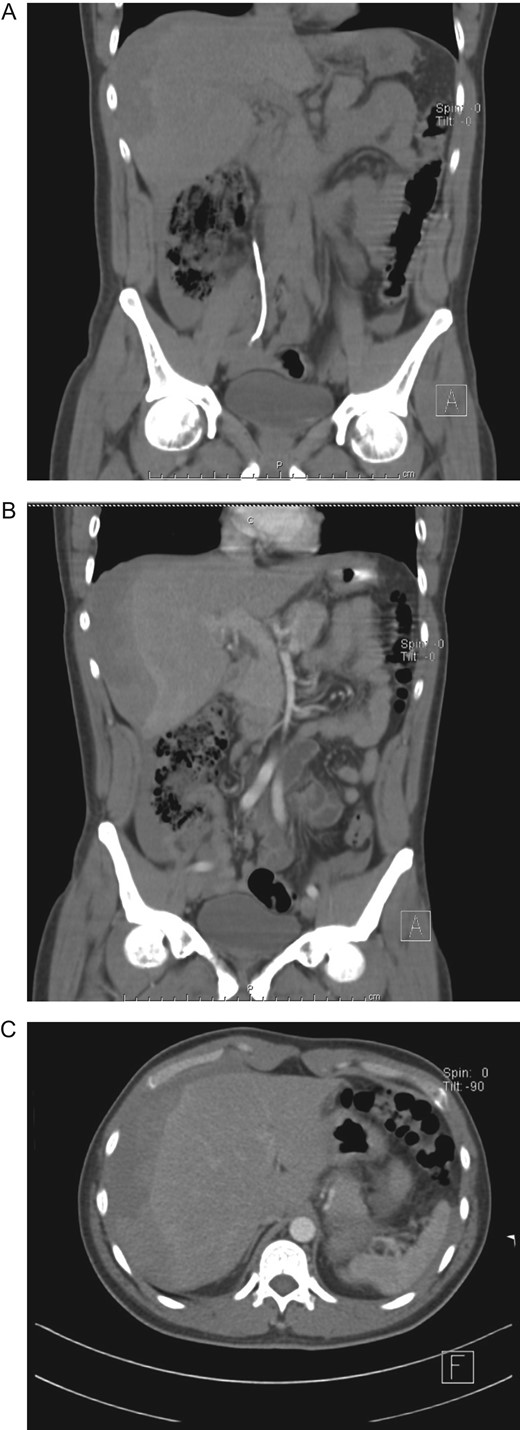
(A) CT, showing double J-stent and hepatic hematoma. (B) Contrast-enhanced CT, revealing a subcapsular liver hematoma. (C) Contrast-enhanced CT, subcapsular liver hematoma without contrast material extravasation.
After adequate resuscitation and analgesia, his pressure and vital signs were stabilized, laboratory exams did not reveal leukocytosis or anemia however his hemoglobin (Hb) level decreased 4 points from 18 to 14 g/dl. He was admitted for close surveillance and under continuous monitoring. During hospitalization, the patient remained stable without tachycardia or episodes of hypotension, his urinary output was normal and his pain disappeared. However, 48 h after admittance, a new CBC revealed a Hb of 10 g/dl, a new CT was performed and the liver hematoma had grown ~50% (Fig. 3A and B), yet as the patient remained stable, non-operative management of his liver hematoma was decided.
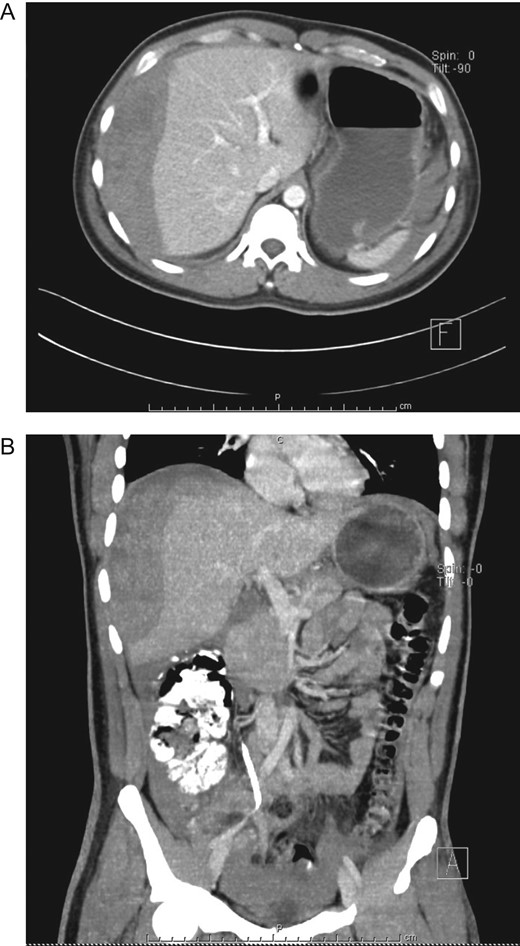
(A) Contrast-enhanced CT, subcapsular liver hematoma 48 h after admittance. (B) Contrast-enhanced CT, the liver hematoma had grown ~50%.
Blood transfusion was not required and after 7 days of conservative therapy, as the patient was completely asymptomatic and his hemoglobin remained stable, he was discharged. On follow-up controls patient is doing well, without any pain, his last Hb was 11 g/dl and a remarkable reduction of the hematoma was seen on a new CT scan.
DISCUSSION
Urolithiasis is one of the most common urological condition and affects up to 12% of the adult population [1], It is mainly caused by diet, changes in lifestyle and undetected underlying diseases [2]. Urolithiasis can be troublesome as these stones can cause severe pain, inflammation, infection, hematuria, kidney deterioration and due to their high prevalence and recurrence a burden for the healthcare system [1, 2].
As with many conditions, multiple treatments have been described for urolithiasis; including ESWL, percutaneous nephrolithotomy, retrograde intrarenal surgery, and conventional open surgery, among others [2].
Since 1982 and its first use by Chaussy et al. ESWL has been a safe and effective non-invasive treatment option for nephrolithiasis as it can achieve an overall stone-free rate up to 75% [3].
ESWL delivers extracorporeal shock energy to the stone and breaks it through various mechanisms; shear force, cavitation, quasi-static squeezing, and dynamic fatigue. This technique was initially thought to be harmless to the kidney and surrounding organs however various complications have been described [3, 4]. Up 7% of the patients who undergo ESWL will develop some kind of mild complication including hematuria, flank pain and urinary tract infection, however, on rare occasions, life-threatening complications can occur [5]. As it happened to our patient. Hepatic hematoma after ESWL is an extremely rare event with few cases ever reported [5, 6]. Clotting disorders, hypertension, diabetes and obesity have been proposed as significant risk factors. The hematomas usually occur from the shock waves themselves, or due to cavitation bubbles in the urine medium that can lead to capillary damage and ultimately renal or subcapsular hemorrhage [6]. Fortunately, most of the times the weight of the blood clot cuts the vessel between the liver parenchyma, and the bleeding usually stops [5].
When a hematoma appears patients usually present with pain that persists despite administrations of analgesics, other symptoms include mild fever and syncope [7]. Diagnosis is challenging as a high index of suspicion is usually needed [7, 8]. Supportive care is the favored treatment for liver hematomas after ESWL, close follow up is vital and blood transfusion should be immediately started when signs of hypovolemic shock are detected [8]. As our patient experienced. Embolization or surgical approaches should be considered in severe cases that do not respond to transfusion and supportive care [7, 9].
ESWL is the most widespread therapy for patients with renal or proximal ureteral lithiasis up to 2 cm in diameter, mainly due to its high success rate and a low complication rate [1, 2]. However, as in any medical procedure complications can occur, a high clinical suspicion is vital since early detection and adequate treatment may prevent potentially fatal outcomes. Close monitoring and follow up is indispensable, as any deviation from the normal course following ESWL should be thoroughly observed.
CONFLICT OF INTEREST STATEMENT
None declared.



