-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandros Poutoglidis, Ioannis Pateras, Vasiliki Kokkinou, Petros Tziolas, Metastatic acinic cell carcinoma of the parotid gland to the abdominal wall, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz109, https://doi.org/10.1093/jscr/rjz109
Close - Share Icon Share
Abstract
Acinic cell carcinoma (ACC) is a low-grade malignant salivary neoplasm. The parotid gland is the predominant site of origin. ACC has a tendency to recur and metastasize, rarely enough to soft tissue as well as other sites. Medical records of a 56-year-old male with a known history of acinic cell carcinoma of the left parotid gland were reviewed. This report aims to highlight the need for early clinical suspicion of the metastatic tendency of parotid gland ACC in patients’ soft tissues, and the vigorous oncologic approach to any suspected metastatic deposits, as this is the standard of practice and only treatment.
INTRODUCTION
Acinic cell carcinoma (ACC) of the salivary gland represents 2.5–5% of all parotid gland neoplasms [1]. Histological grade predicts survival rate more accurate than T and N classifications [2]. Distant metastasis occurs in 12% in ACC patients [3]. Reported metastatic sites include intracranial, lungs, bones, cavernous sinus, spine, sternum, orbit, liver and rarely skin [3–5]. Patients, with localized disease have 5-, 10- and 20-year survival rates of 100%, 99.15% and 94.37%, respectively. Patients with distant metastasis have 5-, 10- and 20-year survival rates of 59.24%, 31.52% and 21.99%, respectively [6], while the type of initial therapy is correlated with prognosis [7]. Limited local excisions, with positive margins, lead to high percentages of recurrence or distant metastasis and so with poor prognosis [8]. Soft tissue involvement as first sign of metachronous metastases is reported in very few cases. Oncologic excision should be performed in any suspicion of a soft tissue metastatic deposit [9].
CASE REPORT
A 56-year-old male was referred in our Hospital’s Emergency Department (ED) with a firm and tender two-month old abdominal wall lump lying underneath the skin, in the subcutaneous fat, resembling an inflamed abdominal cyst.
Patient’s history includes a primary cancer of the left parotid 4 years ago. He underwent a left parotidectomy, with positive margins of resection (R1). Histology confirmed an epithelial neoplasia with a solid acinar cell pattern. Initial oncologic management conducted 25 courses of postoperative radiotherapy. The follow up recommended was six monthly for the first 4 years from initial diagnosis, and remained disease free until his presentation in our ED.
Clinical examination confirmed the mass, which was localized on the left midclavicular, subcostal and lateral to the umbilicus. It was palpable, firm with signs of tenderness. Laboratory tests were normal but clinical suspicion was high and so a computerized tomography (CT) scan with intravenous contrast (IV) was performed. This revealed a 1.8 cm × 2 cm lesion within the subcutaneous fat (Fig. 1), resembling an inflamed cyst.
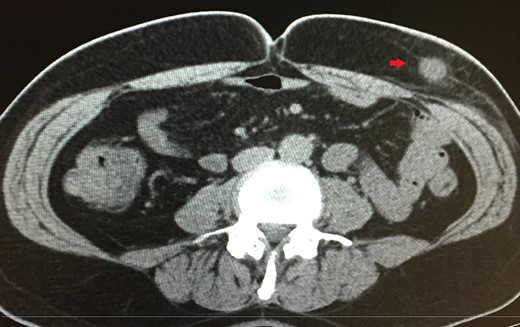
A 1.8 cm × 2 cm lesion (red arrow) revealed in CT scan within the subcutaneous fat.
The patient was given a 7-day course of antibiotics prior to excision. The mass was then oncologically excised under local anesthesia. Histology identified infiltration of fatty abdominal wall tissue from acinic cells cancer and coagulative tumor necrosis, which led to the cystic formation of the lesion (Fig. 2). Immunohistochemistry revealed positive tumor cells for Keratin 8/18, trypsin and Chymotrypsin (Fig. 3). Further follow up scans revealed no metastasis, local recurrence or any other local growth.
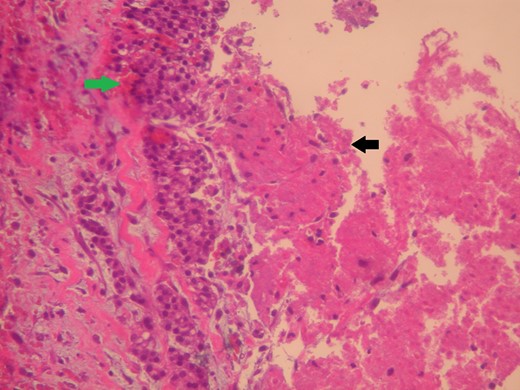
The lesion (green arrow) appears cystic due to its central tumor necrosis (black arrow). Hematoxylin and eosin ×200.
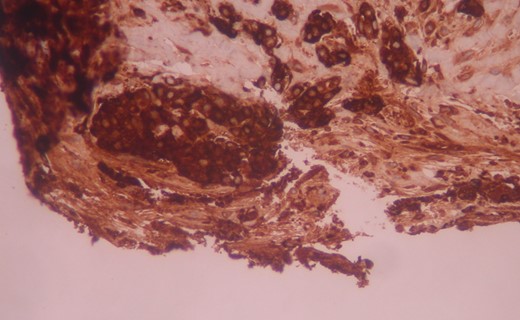
The tumor cells are positive for chymotrypsin in immunohistochemistry. Immunostaining ×200.
Patient did not undergo further treatment and only scheduled for regular three monthly follow up.
DISCUSSION
The standard of care in primary ACC of parotid gland is the complete surgical removal of the tumor, total or subtotal parotidectomy [2]. ACC has generally not been regarded radiosensitive, however patients with an advanced stage or positive resection margins can be given adjuvant postoperative radiotherapy and chemotherapy, for better local tumor control.
Metastatic ACC management is very challenging due to it is rarity and scarce data. Metastasectomy seems to be the most preferable approach for any metastatic deposit [9].
Rare reports similar to our case have been published in the literature. There are cases about mixed tumor, ductal carcinoma and adenocarcinoma of parotid gland that metastized in soft tissue. Varsegi et al. presented in 2008 the first case of widespread cutaneous metastasis from acinic cell carcinoma [4].
Cutaneous/soft tissue metastases from salivary carcinomas are extremely rare [4]. Clinical history is absolutely necessary in reaching a correct diagnosis. When examining subcutaneous or skin lesions of abdominal wall or elsewhere, neoplasms arising from the salivary gland should be regarded as possible sites of origin.
Our case reinforces the empiric knowledge that oncological excision of cutaneous or subcutaneous masses should be performed in every patient with a salivary gland cancer history. There is always a necessity presenting every new similar case in order to conclude in a standard of oncologic management.
CONFLICT OF INTEREST STATEMENT
None declared.



