-
PDF
- Split View
-
Views
-
Cite
Cite
Mohamad Moussa, Mohamed Abou Chakra, Spontaneous cavernosal abscess: a case report and review of literature, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz108, https://doi.org/10.1093/jscr/rjz108
Close - Share Icon Share
Abstract
A cavernosal abscess is a rare condition. It can be idiopathic or with an underlying cause such as intracavernosal injection therapy, foreign bodies, perineal abscesses extension, priapism or trauma. The most common presenting symptoms were penile pain and swelling. Standard treatment consists of drainage via an incision, followed by broad-spectrum antibiotics where some authors describe less invasive techniques such as image-guided aspiration. We present a case of spontaneous left cavernosal abscess diagnosed on MRI in a 60-year-old patient with uncontrolled diabetes mellitus that was treated by percutaneous ultrasound-guided aspiration drainage and systemic antibiotic therapy without any long-term sequela.
INTRODUCTION
Penile abscesses are an uncommon condition [1]. There are multiple etiologies of penile abscesses, including penile injection, traumatic event, cavernosography, priapism and due to undetermined causes [2]. Most cavernosal abscesses are treated with incision and drainage in addition to systemic antibiotics and some cases were successfully treated by aspiration and systemic antibiotic after localization by ultrasonography and MRI. We present a case of spontaneous left cavernosal abscess in a patient with uncontrolled diabetes mellitus treated by percutaneous ultrasound-guided aspiration drainage and systemic antibiotic therapy.The possible etiology, diagnosis and treatment of this rare condition are briefly discussed.
CASE REPORT
A 60-year-old circumcised male with poorly controlled diabetes mellitus Type 2 presented to the outpatient clinic for 10 days history of redness and painful swelling of the distal penile shaft near the base and fever of 39°C associated with dysuria and frequency. The patient denied any recent sexually transmitted disease, trauma, urethral instrumentation or cavernosal injection. His past medical history was unremarkable except for poorly controlled diabetes (last HBA1C of 11.5% (normal: 4–5.6%). Physical examination revealed edema, induration and tenderness in the left proximal penile shaft with no skin breaks. The testicular and epididymal, digital rectal examinations were normal. No dyspnea or a cough or other complaints. Laboratory examination revealed WBCof 14 000/mm3 with left shift,CRP of 102 mg/L, random blood sugar 380 mg/dL, Urine analysis showed 2–3 WBC per high power field, other blood investigations were all within their normal range. He underwent an MRI of the penis that showed a septated and enhancing structure of 2.2 cm in the posterior aspect of the left corpus cavernosum, worrisome for an intracavernosal abscess that impinges on the adjacent urethra (Fig. 1).
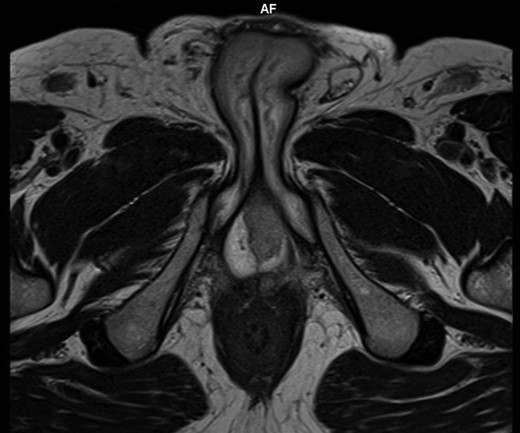
Axial T2 W images of penis showed a well-defined septated area of 2 cm in the posterior aspect of left corpus cavernosum.
Patient was started on broad-spectrum antibiotic (Ertapenem & Vancomycine). Percutaneous ultrasound-guided aspiration drainage was done and pus was drained (Fig. 2) and sent for microscopy, culture and sensitivity.
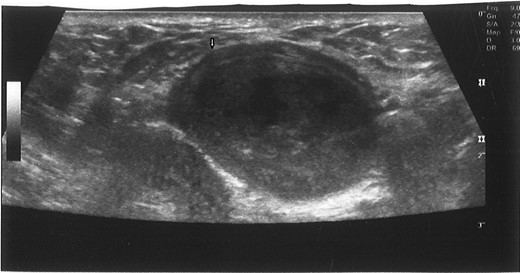
Ultrasound-guided puncture of the mixed echogenic cystic mass of left corpus cavernosum. White arrow: needle entry site.
The culture of the abscess yielded Staphylococcus aureus, the patient was treated by 2 weeks of antibiotic according to the sensitivity test. Blood and urine culture revealed no growth. The Patient was seen in the outpatient clinic 1 week after with only noted a presence of minimal induration with resolution of all symptoms, 1 week later he has been evolving without signs of infection, and he is back to sexual activity. During a follow-up period of 3 months, there was no abscess recurrence.
DISCUSSION
Abscess of the corpus cavernosum is an unusual infection and can develop after trauma, as a complication of cavernosography; after intracavernous injection of vasoactive agents or perineal abscess drainage, intra-abdominal abscess extension and priapism [1, 2]. Spontaneous cavernosal abscess has been described as an abscess without an identifiable underlying cause [3]. The most commonly identified organisms from cultures of cavernosal abscess materials were reported to be S. aureus, Streptococci, Bacteroides and Fusobacteria. Corpus cavernosal abscesses are also associated with diabetes mellitus and other forms of immunosuppression [1]. Corpora cavernosa are resistant to hematogenous dissemination of infection, there have been few reports, one of them about a case where dental caries have been blamed as a cause of penile abscess through hematogenous dissemination [4].
Clinical suspicion of a penile abscess based on local swelling and pain can be confirmed by ultrasound, CT or magnetic resonance imaging (MRI).
Surgical evacuation remains the first line in the treatment of penile abscess followed by systemic antibiotics but, in some cases, there some post-operative complications such as penile deviation, erectile dysfunction or abscess recurrence [1]. Some cases of penile abscess were treated by less invasive interventional techniques (image-guided aspiration with antibiotics) and there was a successful resolution of the abscess without long-term sequela [5, 6]. Regardless of the approach, it is necessary to do a close follow up for the patient, as Ehara et. al. describe a case of 54-year-old patient that underwent open surgical drainage of a cavernosal abscess and 3 weeks later he developed a recurrent abscess with methicillin-resistant S. aureus where he requires total penectomy [7].
In this presented patient, we could not find any causative factor for penile abscess formation; however, uncontrolled diabetes mellitus remains a potential risk factor of our patient. The culture of abscess yielded S. aureus which is a part of the skin microflora; however, the penile skin was not presenting any sign of trauma or abrasion, the inoculation of this bacteria remains unknown. It is important to know, as presented in our case, that single aspiration and appropriate antibiotic could resolve the penile abscess and then avoiding all complications related to open drainage.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
No conflict of interest was declared by the authors.
FUNDING
None.
INFORMED CONSENT
Written and signed informed consent was obtained from the patient.
ETHICAL APPROVAL
Our institution does not require ethical approval for case reports.



