-
PDF
- Split View
-
Views
-
Cite
Cite
Yukihiro Tatekawa, Ileus associated with mesenterium ileocolicum commune: two case reports and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz100, https://doi.org/10.1093/jscr/rjz100
Close - Share Icon Share
Abstract
Two cases of ileus associated with mesenterium ileocolicum commune are reported herein. Case 1 was a 6-year-old girl who was admitted with bilious vomiting and abdominal distension. Plain computed tomography (CT) suggested intestinal volvulus or intussusception. A barium enema revealed an incomplete obstruction or stricture. She underwent a laparotomy. The intra-operative findings revealed midgut volvulus associated with mesenterium ileocolicum commune with normal rotation of the intestine. The volvulus was 180 degrees of counter-clockwise torsion. Case 2 was a 3-year-old boy who was admitted with bilious vomiting. Enhanced CT suggested a duodenal obstruction. A barium meal revealed malrotation and it was difficult to insert an enteral feeding tube into the small intestine. He underwent a laparotomy, and the intra-operative findings revealed Ladd’s bands associated with mesenterium ileocolicum commune and malrotation of the intestine. At present, both patients are doing well and there have been no recurrences.
INTRODUCTION
Mesenterium commune is a type of intestinal malrotation without fixation to the retroperitoneum. Mesenterium commune has no characteristic symptoms, and most cases are noted incidentally during abdominal surgery for complications or other disorders. There are important complications related to mesenterium commune, such as colon volvulus, intussusception, and megacolon. [1–3] One variant of mesenterium commune is referred to as mesenterium ileo-coecale commune because the cecum and the partial portion of the ascending colon share a common loose mesenterium with the intestine. Another variant of mesenterium commune is referred to as mesenterium ileo-colicum commune because the cecum and ascending and right half of the transverse colon share a common loose mesenterium with the intestine. [3]
CASE REPORTS
Two cases of ileus associated with mesenterium ileocolicum commune are reported herein.
Case 1
A 6-year-old girl presented with bilious vomiting and abdominal distension. She has Trisomy 18 and has undergone a tracheostomy and gastrostomy. Abdominal X-ray films showed dilatation of the bowel with gas (Fig. 1a). After injecting contrast medium through the gastostomy, retention of the contrast was noticed, which revealed intestinal obstruction. Based on plain computed tomography (CT) intestinal volvulus or intussusception was suspected (Fig. 1b and c). A barium enema revealed an incomplete obstruction or stricture (Fig. 1d). She underwent a laparotomy, and the intra-operative findings revealed a Meckel’s diverticulum, multiple intestinal tumors that were thought to be ectopic pancreas, and midgut volvulus associated with mesenterium ileocolicum commune and normal rotation of the intestine (Fig. 2a and b). Because of the massive content and gas in the bowel, a tube was inserted into the Meckel’s diverticulum to decompress the intestinal content. The midgut volvulus involved 180 degrees of counter-clockwise torsion, which was released with resection of the Meckel’s diverticulum and an appendectomy. Multiple intestinal tumors were resected, which were indeed diagnosed as ectopic pancreas. At one month post-operatively, she underwent adhesiolysis due to an ileus. She is currently doing well without torsion of the intestines.
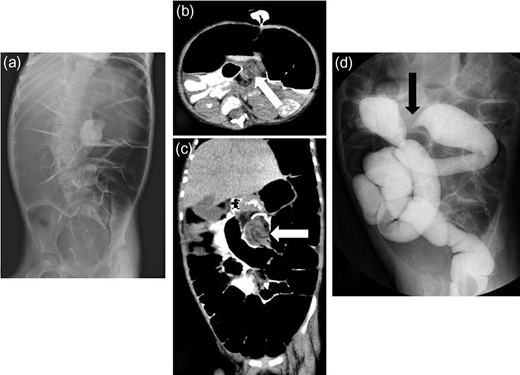
Radiologic findings from Case 1. (a) Abdominal X-ray films showing dilatation of bowel with gas. (b and c) Plain computed tomography showing suspected intestinal volvulus or intussusception (white arrow: suspected lesion). (d) Barium enema revealing an incomplete obstruction or stricture (black arrow: suspected lesion).
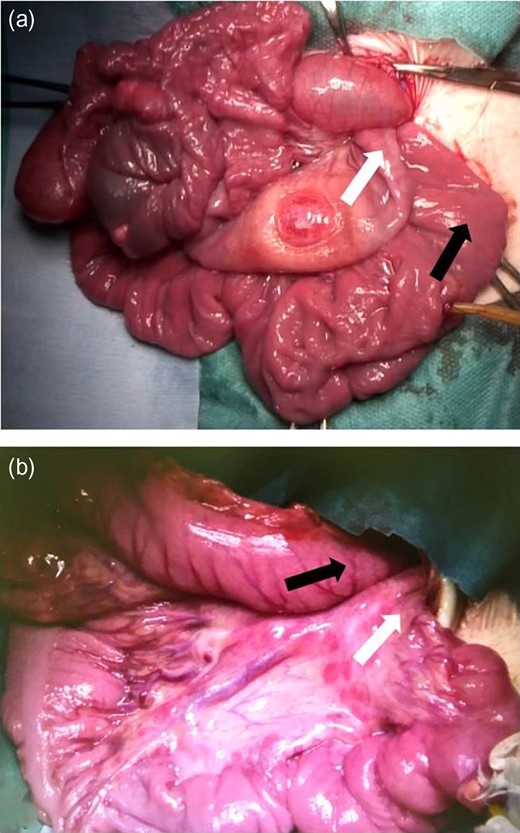
Intra-operative findings from Case 1. (a and b) The findings before releasing the volvulus showing 180 degrees of counter-clockwise torsion and compression of the transverse colon by the intestine (white arrow: oral side, black arrow: anal side). Meckel’s diverticulum and multiple intestinal tumors suspected as ectopic pancreas are shown. The tube was inserted into the Meckel’s diverticulum to decompress the intestinal content.
Case 2
A 3-year-old boy was admitted with bilious vomiting. Abdominal X-ray films showed a gasless abdomen (Fig. 3a). Enhanced CT findings were consistent with duodenal obstruction (Fig. 3b and c). A barium meal revealed malrotation and it was difficult to insert an enteral feeding tube into the small intestine (Fig. 3d). He underwent a laparotomy, and the intra-operative findings revealed Ladd’s bands associated with mesenterium ileocolicum commune and malrotation of the intestine (Fig. 4a and b). He underwent division of the abnormal bands tethering the duodenum, which caused extrinsic compression, widening of the mesenteric base to prevent a further volvulus, and an appendectomy. He is currently doing well without a recurrence.
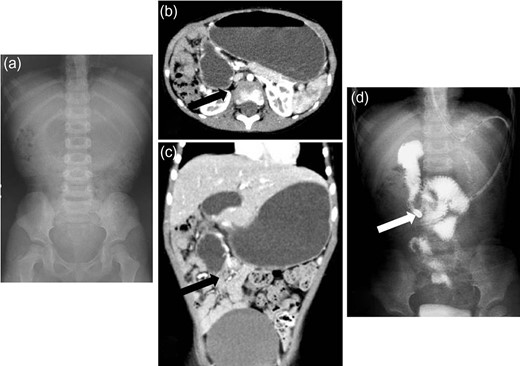
Radiologic findings from Case 2. (a) Abdominal X-ray films showing a gasless abdomen. (b and c) Enhanced CT showing a suspected duodenal obstruction (black arrow: suspected lesion). (d) Barium meal revealing malrotation and difficulty inserting the enteral feeding tube into the small intestine (white arrow: the tip of the tube).
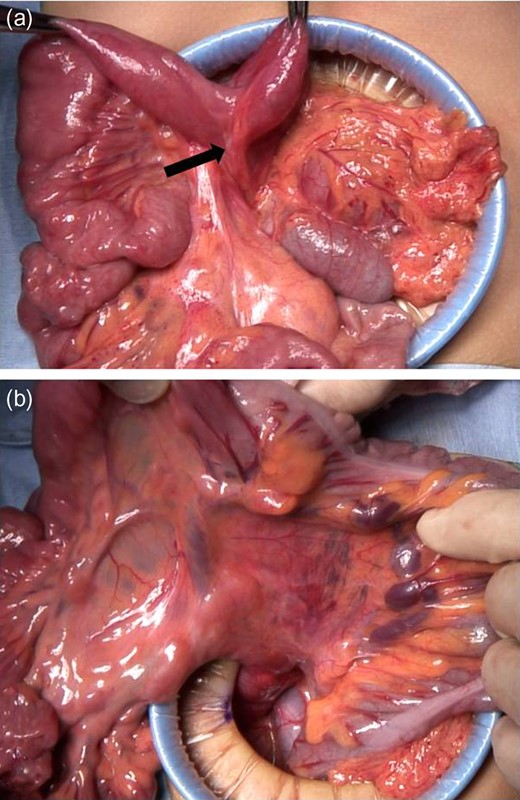
Intra-operative findings from Case 2. (a) The findings showing the abnormal bands tethering the duodenum, which caused extrinsic compression of the duodenum (black arrow: abnormal bands). (b) Mesenterium ileocolicum commune with malrotation of the intestine is shown.
DISCUSSION
During diagnostic evaluation of the volvulus, several reports reported that the contrast medium enema image showed a bird’s beak sign, indicating that the volvulus was located in the intestine or colon. [1–3] The current treatment of choice for uncomplicated colon volvulus is endoscopic release, which is appropriate when there is no peritoneal irritation, rebound tenderness, or intestinal bleeding, and bowel sounds are not absent. [1, 2] Regarding the most appropriate surgical treatment, anchoring the colon and simple reduction or resection of the twisted bowel have been performed. [1–3]
Congenital duodenal obstruction (atresia or stenosis) is associated with various congenital anomalies. [4] If midgut rotation during fetal development is incomplete, the cecum remains in the epigastrium, but the bands fixing the duodenum to the retroperitoneum and cecum continue to form. These congenital extrinsic duodenal bands (Ladd’s bands), extending from the cecum to the lateral abdominal wall and crossing the duodenum, have the potential to cause duodenal obstruction. [5–8] A standard upper gastrointestinal barium series and contrast enema examination showed malposition, but the findings were non-specific. Fundamentally, the treatment for incomplete intestinal rotation is the Ladd procedure, which entails counterclockwise detorsion of the midgut volvulus (if present), division of the abnormal coloduodenal Ladd bands tethering the midgut, which causes extrinsic compression, widening of the mesenteric base to prevent further volvulus, and removal of the malpositioned appendix. [5, 6]
There are important problems to address in treating patients with mesenterium commune. Mesenterium commune has no characteristic symptoms, but as reported in a classic paper involving mesenterium commune with intussusception or volvulus in infants, [2] the patients died on the second day or several hours after surgery. In infants, the intussuscepted or twisted bowel immediately induces circulatory failure or sepsis, and therefore it is necessary to carefully treat infants with suspected intestinal obstruction. Without hesitation, Doppler ultrasonography and enhanced computed tomography, if possible, should be performed. [9, 10]
CONFLICT OF INTEREST STATEMENT
The author has no conflicts of interest. The author alone is responsible for the content and writing of this manuscript.
AUTHOR DISCLOSURE STATEMENT
No competing financial interests or funding exists in connection with this manuscript.



