-
PDF
- Split View
-
Views
-
Cite
Cite
Tikfu Gee, Shu Yu Lim, Nadarajan Sudhakaran, Muhammad Firdaus Hassan, Jejunal interposition for short bowel syndrome in a septuagenarian, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz095, https://doi.org/10.1093/jscr/rjz095
Close - Share Icon Share
Abstract
Short bowel syndrome in adults occurs as a result of massive small intestinal resection commonly due to severe Crohn’s disease, volvulus or tumors. Diarrhea and weight loss are hallmarks of malabsorption which are aggravated if the colon is removed along with the small intestinal resection. Enteral nutrition autonomy is difficult to achieve in such cases of malabsorption where parenteral nutrition are required more often than not. We report a case of short bowel syndrome with severe malabsorption following extensive small bowel removal. The patient eventually underwent intestinal rehabilitation surgery and achieved independence from parenteral nutrition.
INTRODUCTION
Short bowel syndrome develops after the functional length of the small intestines is shortened resulting in malabsorption of water, electrolytes, and nutrients. The anatomical location and the total length of the small intestinal resection affect the functional status of the residual small intestines. Jejunal resection is generally more tolerable than ileal resection. The ileum is able to adapt better and has the potential of replacing the functions of the jejunum. Hence, malabsorption, dehydration and electrolyte imbalances are less pronounced in a patient with an adequate length of residual ileum.
The degree of malnutrition, electrolyte imbalance and dehydration largely depends on the functional residual length of the small intestines. Specialized dietary measures may improve the condition but many patients would eventually require supplementary parenteral nutrition. We report a procedure of anti-peristaltic jejunal interposition performed in a patient with short bowel syndrome.
CASE REPORT
A 70-year-old Caucasian lady was transferred to our hospital following a massive small intestinal resection and right hemicolectomy due to an intestinal obstruction. Cancer of the right colon with the involvement of the proximal ileum was found during the surgery. The surgeon went on to perform a right hemicolectomy and resection of the entire ileum. A jejunum stoma was created with the colon closed up like a Hartmann’s procedure.
Following a clinical reassessment of the patient, a synchronous cancer of the sigmoid colon was discovered. This finding was missed during the first surgery. Hence, this patient had to undergo an anterior resection and completion of colectomy. Consequently, she ended up with a permanent jejunostomy without any remaining colon. During the second surgery, the jejunostomy was measured and found to be ~150 cm from the duodenojejunal flexure.
The jejunostomy output was high and the patient was consistently losing weight and had suffered significant fluid and electrolyte imbalances. Several attempts were made to customize her dietary requirements such as oral nutrition supplement with a peptide-based semi-elemental formula; modified diet to increase protein, fiber and salt intake; parenteral nutrition with added mirconutrients; pharmacological agents such as high dose loperamide, anticholinergic drugs, oral rehydration solutions and even octreotide were used to reduce stoma output but to no success.
After 6 months of a failed conservative approach to treat her malabsorption, a collective decision was made to find a surgical solution for the short bowel syndrome. After going through various intestinal rehabilitation surgical options, jejunal interposition was decidedly acceptable as the best procedure for the patient.
Surgical technical details
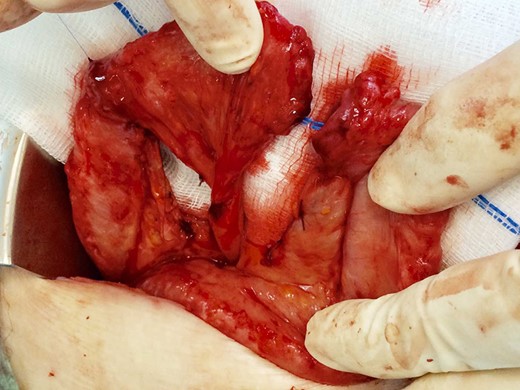
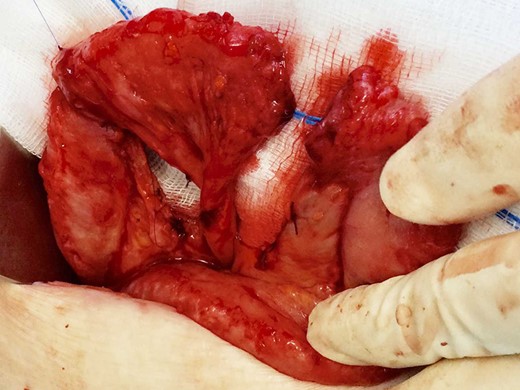
A 10 cm segment of jejunum measuring ~20 cm distal to the stoma was identified. The mesentery is also divided in a ‘V’ shaped manner towards the main blood supply (Fig. 1). The mesentery along with the jejunal segment is twisted 180° and the ends transposed (Fig. 2). The anastomosis on each end is made using interrupted absorbable 5-0 polyglactin sutures. The mesenteric defects are approximated with absorbable 4-0 sutures (Fig. 3). This divided segment of the jejunum now becomes an anti-peristaltic portion of the intestines which could be evidently seen intra-operatively (Fig. 4). The patient recuperated well in the postoperative period and was discharged following a week of supplemental parenteral nutrition.

Division of a segment of jejunum and its mesentery, preserving the main blood supply.
The divided segment of jejunum twisted 180° along its mesenteric axis.
After ensuring adequate perfusion, proximal ends of the interposed jejunum were anastomosed.
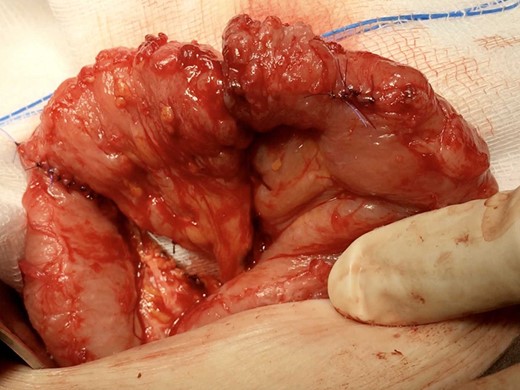
Completion of the jejunal interposition with closure of the mesentery with non-absorbable sutures.
The stoma output was remarkedly reduced, and she could tolerate food better. She did not gain significant weight while she was receiving artificial nutrition support, but she did not lose more weight since the surgery. Her electrolyte levels were also normalized and her urine output improved. Her colorectal cancer was considered cured as the resected margins were clear and the lymph status were negative for cancer.
DISCUSSION
The management of short bowel syndrome requires a multidisciplinary approach in which the fluids and nutritional support are customized according to the degree of malnutrition, length and type of the residual intestines and presence of remnant colon. The mainstay of management of short bowel syndrome includes parenteral nutrition and dietary adjustments until a degree of intestinal adaptation has been achieved. However, patients receiving long-term parenteral nutrition are at risk of developing catheter-related complications, bone disease, cholelithiasis or liver failure [1]. Furthermore, parenteral nutrition limits the patients’ activities, be it social or work.
Because of these parenteral nutrition-related comorbidities, numerous surgical procedures have been devised for patients in whom non-operative treatments have failed as well as to enable parenteral nutrition weaning. Intestinal rehabilitation surgery may be necessary in some cases of short bowel and these can be classified into three subgroups of operations including bowel lengthening surgery, procedures that prolong intestinal transit and bowel transplantation [2]. The jejunal segment considered for the interposition should be as distal or as near to the stoma as possible. The anti-peristaltic segment is more effective when placed distally so that there will be a longer transit time for as much chyme as possible in the proximal intestines. By converting a section of the jejunum as distal as possible, an attempt is made to push back of the intestinal contents in order to increase more time for the intestinal content to undergo the process of digestion and absorption.
In this patient, neither bowel lengthening nor bowel transplantation was considered as the remnant intestines were still around 150 cm of jejunum. The jejunal interposition was deemed the most suitable procedure as her main issue was the short intestinal transit time. Surgical reconstruction of the residual small bowel using anti-peristaltic jejunal segments have been recommended for patients with resected ileum and ileocaecal valve [3]. This anti-peristaltic segment creates a partial mechanical obstruction thus prolong the transit time and enhance nutrient absorption [3]. The anti-peristaltic segment causes a reversed peristalsis hence disrupting the motility of the proximal intestine resulting in a delay of myoelectrical activity in the distal segment [4].
The suggested reversed segment lengths of 10–15 cm are recommended for adults and ~3 cm for children to provide maximum benefit of delaying the transit time [4]. Short segments may be inefficient in slowing transit time whereas longer segments may create bowel obstruction syndrome [4]. Hence, a careful balance of the interposed bowel segment would need to be achieved. In a case series reported by Panis et al. [5], it was found that the ideal reversed segment length for an adult is 10 cm. The main limitation of this surgery is that the surgery is only proved feasible if remnant small bowel was at least ≥25 cm long [5]. Anti-peristaltic jejunal interposition is a good option in the treatment of short bowel syndrome with a short intestinal transit time but a considerable adequate residual bowel length.
CONFLICT OF INTEREST STATEMENT
There is no personal or financial conflict of interest.
DECLARATIONS
Consent for publication: Written informed consent was obtained from the patient for publication of this case report.
FUNDING
The study was funded internally with no external support for the research or the writing of the article.
REFERENCES
- weight reduction
- parenteral nutrition
- crohn's disease
- diarrhea
- enteral nutrition
- malabsorption syndrome
- adult
- intestine, small
- intestines
- short bowel syndrome
- surgical procedures, operative
- colon
- neoplasms
- rehabilitation
- surgery specialty
- small-intestine resection
- intestinal volvulus
- jejunal interposition
- symptom aggravating factors



